Device Portfolio
Browse some of the medical training devices that were created in the Innovations Laboratory:
Synthetic Simulators

Neonate Chest Tube
The simulator provides trainees with the opportunity to practice the technically detailed — but common — procedure of chest tube placement for newborn infants. This simulator was built using 3D printing technology coupled with realistic synthetic material, allowing creation of a low-cost, reusable and easily reproducible simulator.
Collaborator: Arika Gupta, MD, Neonatology, Ann & Robert H. Lurie Children’s Hospital of Chicago
Pediatric Surgery
These synthetic models are the world’s first validated simulators for the surgical repair of tracheoesophageal fistula, duodenal atresia, diaphragmatic hernia and surgical gastrostomy tube placement. Each simulator can be used for traditional open and minimally invasive procedural training.
Collaborator: Katherine A. Barsness, MD, Pediatric Surgery, Ann & Robert H. Lurie Children’s Hospital of Chicago
Featured at: International Pediatric Endosurgery Group (IPEG) and World Federation of Associations of Pediatric Surgeons (WOFAPS) conferences, 2012 and 2013 respectively

Facial Laceration
This simulator is used to teach facial wound closure techniques. It is a low-cost and portable model that’s made using synthetic materials to maintain more realistic elasticity of the skin as compared to cadaver models.
Collaborator: Amy L. Halverson, MD, colon and rectal surgeon, Feinberg School of Medicine, Northwestern University
Featured at: American College of Surgeons Rural Surgery Symposium and Skills Course, 2012
Melanoma Model
This simulator is used in primary care training on how to distinguish possible melanoma from benign lesions. It incorporates sensor technologies to track learning through computerized data collection.
Collaborator: June K. Robinson, MD, Dermatology, Feinberg School of Medicine, Northwestern University


Thyroid Trainer
This simple tool allows trainees to practice using ultrasound for fine-needle aspiration biopsies targeting thyroid abnormalities.
Collaborator: Cord Sturgeon, MD, associate professor in Surgery, Gastrointestinal and Endocrine, Northwestern University Feinberg School of Medicine
Featured at: Thyroid and Parathyroid Ultrasound Course and the World Congress on Thyroid Cancer, 2013; International Society of Endocrinology and the Endocrine Society: ICE/ENDO, 2014
Hybrid Simulators

Pediatric Surgery
These hybrid simulators are adaptations of a synthetic pediatric surgery simulator that uses real tissue to replicate surgical anatomy for complex operative procedures. Models include surgical repair of tracheoesophageal fistula, duodenal atresia, diaphragmatic hernia and lobectomy. Each simulator can be used for traditional open and minimally invasive procedural training.
Collaborator: Katherine A. Barsness, MD, Pediatric Surgery, Ann & Robert H. Lurie Children’s Hospital of Chicago
Cricothyrotomy Trainer
This hybrid simulator incorporates real tissue and a synthetic base to accurately replicate the anatomy associated with performing an emergency cricothyrotomy.

Other Educational Models
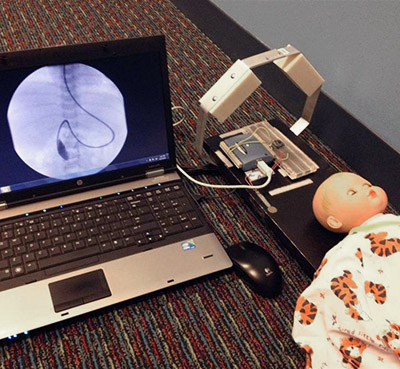
Pediatric Fluoroscopy Trainer
This training tool simulates the interface that physicians interact with while performing fluoroscopy on pediatric GI patients. It incorporates the use of accelerometers and force-sensitive resistors to transmit data to a computer program.
Collaborator: Ellen C. Benya, MD, Radiology, Ann & Robert H. Lurie Children’s Hospital of Chicago
Connect with the Innovations Lab
Recognize an education gap that the Innovations Lab can help you meet?
We want to work with you.