Our Research Impact
Cutting-Edge Research with Real-World Impact
At the Simpson Querrey Lung Institute for Translational Science (SQLIFTS), we pursue high-impact research with the ultimate goal of improving patient care and saving lives in Chicago and beyond. Our work is motivated by patients like Trupti Patel, who faced a rare lung cancer diagnosis with two options: clinical trial or nothing. For National Cancer Survivors Day, she explained her lifesaving decision.
Trupti's story is just one example of the direct impact of research at SQLIFTS. Although institutional grants and generous private donations are vital to the success of our work, it would not be possible without support from federal contracts. But for patients and their loved ones, the true value of our research is incalculable.
Read on to learn more about our research impact here at SQLIFTS.
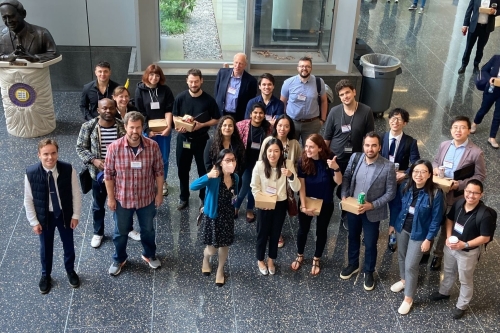
Global Voices in Patient-Centered Research
Introducing Global Voices in Patient-Centered Research, a new conference series highlighting how research transforms lives.
Focus on Cystic Fibrosis
Our inaugural session kicked off with a focus on cystic fibrosis. Speakers included cystic fibrosis clinicians Manu Jain, MD and Susanna McColley, MD at Northwestern, JP Clancy, MD, Senior Vice President of Clinical Research at the Cystic Fibrosis Foundation, and a patient living with cystic fibrosis.
To read a transcript of this video, please click here.
This conference is sponsored by Northwestern University, the University of Pittsburgh, and the German Centers for Lung Research. Please check back again soon for updates on future events in this series.
A Research Success Story, Still in Progress
Research funded by the National Institutes of Health (NIH) is enabling children with cystic fibrosis to become healthy adults. The disease is fatal in early childhood without effective treatment, and for many decades effective treatment was limited to management of symptoms. Most patients with cystic fibrosis did not survive past their mid-thirties.
But the outlook changed dramatically in 1989 with the discovery of CFTR, the gene responsible for cystic fibrosis. With understanding of the genetic basis of cystic fibrosis, research into CFTR mutations and their effects on the CFTR protein accelerated. In 2012 the first CFTR modulator was approved by the Food and Drug Administration (FDA) to treat cystic fibrosis. Other drug approvals followed, and still more therapies are in clinical trials or preclinical development.
At SQLIFTS, our continuous NIH-funded research has supported our leadership in clinical trials of these new therapies and better treatment options for our patients in the Adult Cystic Fibrosis Program at Northwestern. These new medications, which would not exist without NIH-supported research, have transformed the lives of patients with cystic fibrosis. SQLIFTS researchers have also developed a new wireless sweat patch that measures sweat chloride concentrations, which would allow for remote monitoring of a patient's response to medication and improve clinical decision-making about these treatments.
Thanks to such NIH-funded advancements in both basic and clinical research, many people with cystic fibrosis now can consider the option to have children of their own, leading to a recent "baby boom" among patients. And with improvements in life expectancy, clinicians have turned to aging and cystic fibrosis as a new research priority.
But the story is far from over. The current FDA-approved CFTR modulators are not cures. Patients with cystic fibrosis who take these medications still face exacerbations, complications, and side effects from these and other drugs. Further research is still needed to better understand the biology of cystic fibrosis and help the patients who live with it.
Patient Stories: DREAM Program
The Northwestern Medicine DREAM Program (Double Lung Transplant Registry Aimed for Lung-Limited Malignancies, clinical trial registry number NCT05671887) is just one example of federally funded research at SQLIFTS making an impact on patients’ lives. Here is the story of Cornelia Tischmacher, another patient with lung cancer who made a lifesaving decision.
A Mother’s Journey for a Second Chance at Life
 In January 2018, eight months after giving birth to twins, Cornelia Tischmacher of Berlin, Germany, saw a doctor for a case of pneumonia that would not go away. The 40-year-old art historian and gallerist, who was healthy, worked out, and did not smoke, was shocked when tests showed she had stage 3 lung cancer. To do everything she could to stay alive for her children, Tischmacher underwent surgery and chemotherapy in June 2018.
In January 2018, eight months after giving birth to twins, Cornelia Tischmacher of Berlin, Germany, saw a doctor for a case of pneumonia that would not go away. The 40-year-old art historian and gallerist, who was healthy, worked out, and did not smoke, was shocked when tests showed she had stage 3 lung cancer. To do everything she could to stay alive for her children, Tischmacher underwent surgery and chemotherapy in June 2018.
 But by October 2019, Tischmacher’s cancer had returned. Doctors recommended palliative care, and by June 2024 she could no longer breathe without supplemental oxygen. That is when she discovered Northwestern’s DREAM Program, in which select patients with advanced lung cancers confined to the lungs are considered for a double-lung transplant. Tischmacher had telehealth visits with Ankit Bharat, MD, chief of thoracic surgery and director of the Canning Thoracic Institute and of the SQLIFTS Translational Innovation Program.
But by October 2019, Tischmacher’s cancer had returned. Doctors recommended palliative care, and by June 2024 she could no longer breathe without supplemental oxygen. That is when she discovered Northwestern’s DREAM Program, in which select patients with advanced lung cancers confined to the lungs are considered for a double-lung transplant. Tischmacher had telehealth visits with Ankit Bharat, MD, chief of thoracic surgery and director of the Canning Thoracic Institute and of the SQLIFTS Translational Innovation Program.
 Tischmacher was accepted to the DREAM Program. In December 2024 she boarded an air ambulance and flew from Berlin to Chicago. She was admitted to the intensive care unit (ICU) at Northwestern Memorial Hospital and placed on the transplant waiting list on Christmas Eve. Two days after being listed, Tischmacher received new lungs.
Tischmacher was accepted to the DREAM Program. In December 2024 she boarded an air ambulance and flew from Berlin to Chicago. She was admitted to the intensive care unit (ICU) at Northwestern Memorial Hospital and placed on the transplant waiting list on Christmas Eve. Two days after being listed, Tischmacher received new lungs.
 Tischmacher must remain in Chicago near her medical team for the year following her transplant procedure. However, her husband, Udo Kittelmann, and their 8-year-old twins, Leo and Lucie, are remaining in Berlin for the twins’ schooling. Being far from her family has been difficult for Tischmacher, but in April 2025 the whole family finally met for a joyful reunion in Chicago. It was the twins’ first time visiting their mother since she had flown from Berlin in December.
Tischmacher must remain in Chicago near her medical team for the year following her transplant procedure. However, her husband, Udo Kittelmann, and their 8-year-old twins, Leo and Lucie, are remaining in Berlin for the twins’ schooling. Being far from her family has been difficult for Tischmacher, but in April 2025 the whole family finally met for a joyful reunion in Chicago. It was the twins’ first time visiting their mother since she had flown from Berlin in December.
Read more about Tischmacher’s story at Northwestern Medicine Newsroom.
Striving to Save Lives and Improve Outcomes
 Lung transplant patients at Northwestern and their loved ones have been directly impacted by research funded by the National Institutes of Health (NIH), which supports physicians and scientists seeking to improve outcomes after lung transplantation. Our research has led us to develop new approaches such as “lungs in a box” and “lungs in a fridge” to more efficiently use donated organs. Historically, only 20% of lungs that were donated were used for transplantation. We have more than tripled that number so more patients have access to this lifesaving treatment. In addition, most of our patients now wait less than one week for an organ, and very few die before one becomes available.
Lung transplant patients at Northwestern and their loved ones have been directly impacted by research funded by the National Institutes of Health (NIH), which supports physicians and scientists seeking to improve outcomes after lung transplantation. Our research has led us to develop new approaches such as “lungs in a box” and “lungs in a fridge” to more efficiently use donated organs. Historically, only 20% of lungs that were donated were used for transplantation. We have more than tripled that number so more patients have access to this lifesaving treatment. In addition, most of our patients now wait less than one week for an organ, and very few die before one becomes available.
 Findings from our research program have also allowed us to offer transplantation to patients like Tischmacher with lung cancer that is too advanced for standard surgical therapy and to patients who have been cured from a recent cancer. In the past year, more than 40 patients from around the world have benefited from this procedure. The success of our research program enabled the Northwestern Medicine Canning Thoracic Institute to perform the highest number of lung transplants in the United States in 2024.
Findings from our research program have also allowed us to offer transplantation to patients like Tischmacher with lung cancer that is too advanced for standard surgical therapy and to patients who have been cured from a recent cancer. In the past year, more than 40 patients from around the world have benefited from this procedure. The success of our research program enabled the Northwestern Medicine Canning Thoracic Institute to perform the highest number of lung transplants in the United States in 2024.
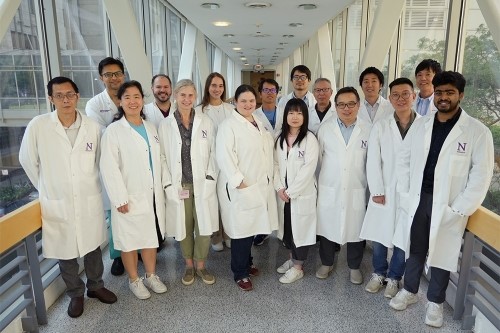
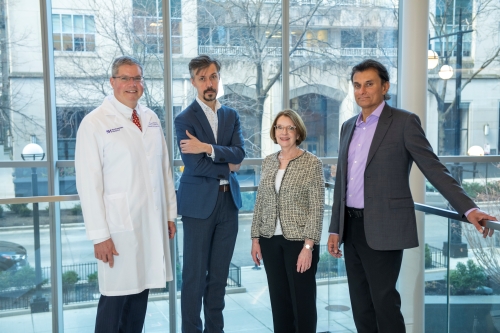
Teamwork Makes DREAM Work
 Healthcare is a team effort, especially in a field as complex as lung transplantation. Tischmacher and other patients in the DREAM Program get to know Dr. Bharat and members of the lung transplant team at the Canning Thoracic Institute. But the work of the DREAM program is also supported behind the scenes by another team, one of researchers.
Healthcare is a team effort, especially in a field as complex as lung transplantation. Tischmacher and other patients in the DREAM Program get to know Dr. Bharat and members of the lung transplant team at the Canning Thoracic Institute. But the work of the DREAM program is also supported behind the scenes by another team, one of researchers.
 At SQLIFTS, Bharat leads investigators in our lung transplantation project, funded by a program project grant awarded by NIH to dissect the molecular mechanisms of rejection to improve the lives of lung transplant recipients. Other NIH grants have supported innovative preclinical findings by Bharat and his laboratory, such as the discovery of a surprising connection between COVID-19 and cancer regression. Although these and other recent discoveries are still at early stages, they pave the way for future innovations in the clinic that will help patients like Cornelia Tischmacher.
At SQLIFTS, Bharat leads investigators in our lung transplantation project, funded by a program project grant awarded by NIH to dissect the molecular mechanisms of rejection to improve the lives of lung transplant recipients. Other NIH grants have supported innovative preclinical findings by Bharat and his laboratory, such as the discovery of a surprising connection between COVID-19 and cancer regression. Although these and other recent discoveries are still at early stages, they pave the way for future innovations in the clinic that will help patients like Cornelia Tischmacher.
Lung Cancer on the Rise in Young Women
 Lung cancer is the leading cause of cancer-related deaths in the United States, and doctors have noticed a startling new trend. Says Bharat, “On a daily basis, we’re seeing more young women being diagnosed with lung cancer. Conventionally, lung cancer has been associated with smoking and older age. While smoking certainly increases your chances of developing lung cancer, we’re seeing an explosion of lung cancer cases in patients who have never smoked or had limited smoking exposure—like Cornelia. The majority of them are young, and the majority are women, and we still aren’t sure why this is happening.” Hence, the Canning Thoracic Institute has started several research programs to try and understand why more women are being diagnosed with lung cancer.
Lung cancer is the leading cause of cancer-related deaths in the United States, and doctors have noticed a startling new trend. Says Bharat, “On a daily basis, we’re seeing more young women being diagnosed with lung cancer. Conventionally, lung cancer has been associated with smoking and older age. While smoking certainly increases your chances of developing lung cancer, we’re seeing an explosion of lung cancer cases in patients who have never smoked or had limited smoking exposure—like Cornelia. The majority of them are young, and the majority are women, and we still aren’t sure why this is happening.” Hence, the Canning Thoracic Institute has started several research programs to try and understand why more women are being diagnosed with lung cancer.
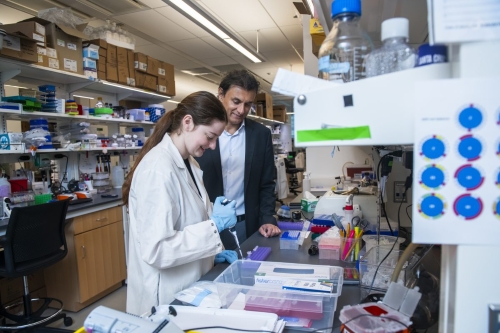
Working to Understand the Biology of Cancer
 Meanwhile in the laboratory, researchers at SQLIFTS and across Northwestern work tirelessly to understand the biology of cancer. Navdeep Chandel, PhD, director of the SQLIFTS Discovery Program, leads a laboratory dedicated to discovering new biology linked to mitochondria and metabolism that controls physiological responses and diseases including cancer. Chandel led research demonstrating that metformin, a widely used diabetes drug, inhibits cancer growth. More recently, Chandel and his research group have discovered that metformin lowers blood sugar by interfering with mitochondria. NIH-funded research directed by Chandel has opened an entirely new area of therapies to treat a host of cancers by targeting their vulnerable metabolic machinery. These contributions were recognized by his receipt of the 2023 Lurie Prize in Biomedical Sciences.
Meanwhile in the laboratory, researchers at SQLIFTS and across Northwestern work tirelessly to understand the biology of cancer. Navdeep Chandel, PhD, director of the SQLIFTS Discovery Program, leads a laboratory dedicated to discovering new biology linked to mitochondria and metabolism that controls physiological responses and diseases including cancer. Chandel led research demonstrating that metformin, a widely used diabetes drug, inhibits cancer growth. More recently, Chandel and his research group have discovered that metformin lowers blood sugar by interfering with mitochondria. NIH-funded research directed by Chandel has opened an entirely new area of therapies to treat a host of cancers by targeting their vulnerable metabolic machinery. These contributions were recognized by his receipt of the 2023 Lurie Prize in Biomedical Sciences.
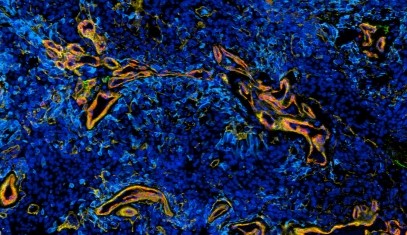
 Karen Ridge, PhD, director of the SQLIFTS Health Education Program and core leader of the lung transplantation project, has also published research in Oncogene on non–small cell lung cancer. This publication authored by Ridge and members of her laboratory was supported by multiple grants awarded by NIH. Ridge’s funding includes the program project grant for the SQLIFTS lung regeneration project, which she leads. Services were provided by essential core research facilities funded by both indirect costs and grants of their own. And Alexandra Berr, PhD, and Kristin Wiese, MD, were supported by the Division of Pulmonary and Critical Care’s T32 training grant, also directed by Ridge. This federally funded program has trained and supported many physicians at Canning Thoracic Institute and many more throughout the United States. To learn more, please read the section below on the T32 Lung Science Training Program.
Karen Ridge, PhD, director of the SQLIFTS Health Education Program and core leader of the lung transplantation project, has also published research in Oncogene on non–small cell lung cancer. This publication authored by Ridge and members of her laboratory was supported by multiple grants awarded by NIH. Ridge’s funding includes the program project grant for the SQLIFTS lung regeneration project, which she leads. Services were provided by essential core research facilities funded by both indirect costs and grants of their own. And Alexandra Berr, PhD, and Kristin Wiese, MD, were supported by the Division of Pulmonary and Critical Care’s T32 training grant, also directed by Ridge. This federally funded program has trained and supported many physicians at Canning Thoracic Institute and many more throughout the United States. To learn more, please read the section below on the T32 Lung Science Training Program.
Essential Research Saves Lives
 For Cornelia Tischmacher, all of this research has culminated in a priceless opportunity to live her life and spend more time with her children. “Seeing my children for the first time in four months was absolutely wonderful. The weight of my illness had weighed them down, and to see me healthy again was overwhelming—but in a good way,” said Tischmacher. “It’s a happy continuation of the story because it could have been so different. When we said our initial ‘goodbyes’ in December, it was much more dramatic because we didn’t know how things would go.”
For Cornelia Tischmacher, all of this research has culminated in a priceless opportunity to live her life and spend more time with her children. “Seeing my children for the first time in four months was absolutely wonderful. The weight of my illness had weighed them down, and to see me healthy again was overwhelming—but in a good way,” said Tischmacher. “It’s a happy continuation of the story because it could have been so different. When we said our initial ‘goodbyes’ in December, it was much more dramatic because we didn’t know how things would go.”
Tischmacher’s incredible journey and heartwarming reunion have been covered by the Chicago Sun-Times, CBS News Chicago, WBEZ Chicago, Euronews Health, and HealthDay News. Her story and those of other patients whose lives have been saved are the ultimate motivation for our work at SQLIFTS—research made possible by federal funding.
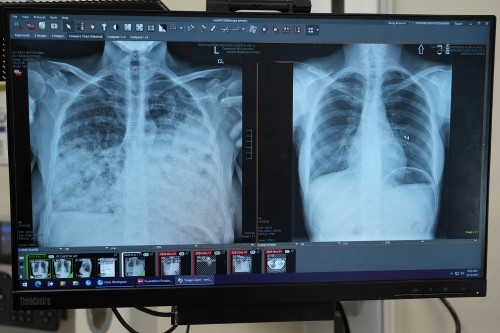
Patient Stories: Lung Health Center
In a new study published in JAMA Network Open, SQLIFTS researchers led by Ankit Bharat, MBBS discovered that of nearly 1,000 consecutive patients treated for lung cancer at Northwestern Medicine, only 35% would have qualified for screening according to the criteria set by the U.S. Preventive Services Task Force. The two-thirds of patients who would have been excluded were disproportionately women and never-smokers.
“'A majority of the lung cancer patients in this country would not meet the screening criteria as it exists currently,” said Bharat in The Washington Post. “'If we have a more broader screening program, similar to breast and colon, then we would be able to detect substantially more patients at earlier stage.'” Bharat also appeared on nationally on NBC News and on ABC7 Chicago to discuss these findings and their implications.
In response to these findings, Northwestern Medicine has launched the Lung Health Center at the Canning Thoracic Institute to detect lung, heart, and bone conditions earlier. Universal age-based screening would help patients such as Danielle Hoeg and Carla Tapia, young mothers who were diagnosed with lung cancer. Learn more about their stories, the Lung Health Center, and the research that set it in motion at Northwestern Medicine Newsroom.
Super-SCRIPT Center
The Super-SCRIPT (Successful Clinical Response In Pneumonia Therapy, SCRIPT²) Systems Biology Center, a cooperative agreement research program funded by the National Institutes of Health (NIH), aims to advance our understanding of severe pneumonia. This work has revolutionized the treatment of pneumonia for patients in the intensive care unit (ICU).
An Innovative, Systems Biology Approach
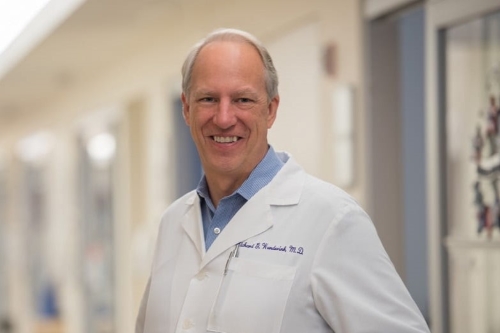 Led by Richard Wunderink, MD, SCRIPT² combines cutting-edge multi-omics technologies, clinical measurements, and machine learning to explore the complex interactions between humans and pathogens that influence the course of pneumonia in patients in the ICU. With a focus on both community-acquired pneumonia and hospital-acquired/ventilator-associated pneumonia, the center seeks to identify biomarkers and therapies that can improve patient outcomes and help physicians in the ICU decide on the best treatment for each patient.
Led by Richard Wunderink, MD, SCRIPT² combines cutting-edge multi-omics technologies, clinical measurements, and machine learning to explore the complex interactions between humans and pathogens that influence the course of pneumonia in patients in the ICU. With a focus on both community-acquired pneumonia and hospital-acquired/ventilator-associated pneumonia, the center seeks to identify biomarkers and therapies that can improve patient outcomes and help physicians in the ICU decide on the best treatment for each patient.
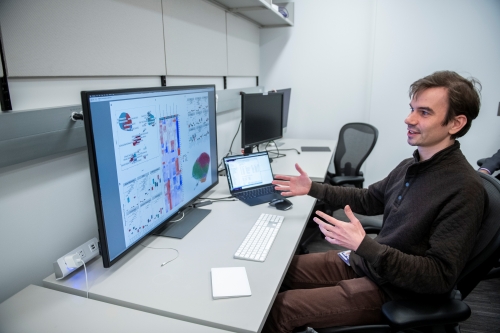
Machine Learning Reveals Patterns in the Data
 SCRIPT Tech Core lead and project co-investigator Benjamin Singer, MD, was senior author of a SCRIPT Center study published in the Journal of Clinical Investigation in which machine learning was applied to clinical data from patients in the ICU to search for patterns predicting poor outcomes. Singer and the SCRIPT researchers found that secondary pneumonia drove many COVID-19 deaths among critically ill patients in the ICU who required mechanical ventilation, not the overwhelming inflammation that had initially believed to have been responsible.
SCRIPT Tech Core lead and project co-investigator Benjamin Singer, MD, was senior author of a SCRIPT Center study published in the Journal of Clinical Investigation in which machine learning was applied to clinical data from patients in the ICU to search for patterns predicting poor outcomes. Singer and the SCRIPT researchers found that secondary pneumonia drove many COVID-19 deaths among critically ill patients in the ICU who required mechanical ventilation, not the overwhelming inflammation that had initially believed to have been responsible.
 This publication was funded by multiple grants awarded by NIH, in addition to that for the SCRIPT research program. For example, co-first-author Catherine Gao, MD, was supported by the Division of Pulmonary and Critical Care’s T32 training grant, directed by SQLIFTS Health Education Program director and lung regeneration project leader Karen Ridge, PhD. (To learn more about this crucial federally funded training program, please see the section below on the T32 Lung Science Training Program.)
This publication was funded by multiple grants awarded by NIH, in addition to that for the SCRIPT research program. For example, co-first-author Catherine Gao, MD, was supported by the Division of Pulmonary and Critical Care’s T32 training grant, directed by SQLIFTS Health Education Program director and lung regeneration project leader Karen Ridge, PhD. (To learn more about this crucial federally funded training program, please see the section below on the T32 Lung Science Training Program.)
Singer’s funding for his laboratory includes the program project grant for the SQLIFTS lung aging project and the program project grant for the lung regeneration project, on which he is a sub-project leader. Co-senior author Alexander Misharin, MD, PhD, director of the SQLIFTS Technology Program, is also supported by these and other grants from NIH. And co-senior-author Scott Budinger, MD, director of SQLIFTS and leader of the lung aging project, also receives funding from the Department of Veterans Affairs for research in his laboratory.
"Proof of Principle, Rapid Translation"
 The insights from this federally funded study have subsequently informed treatment decisions made by physicians caring for mechanically ventilated patients in the ICU at Northwestern and beyond. As Singer told ABC7 Chicago, “We've learned a lot [about] how to take care of these patients once they come into hospital and ICU, what medications to give, what medications not to give.” Reflecting on the experience, he later told new Feinberg members of the AOA Medical Honor Society, “This is proof of principle, rapid translation and also a story about humility. Revaluating your assumptions, revaluating and learning from the data that you generated.”
The insights from this federally funded study have subsequently informed treatment decisions made by physicians caring for mechanically ventilated patients in the ICU at Northwestern and beyond. As Singer told ABC7 Chicago, “We've learned a lot [about] how to take care of these patients once they come into hospital and ICU, what medications to give, what medications not to give.” Reflecting on the experience, he later told new Feinberg members of the AOA Medical Honor Society, “This is proof of principle, rapid translation and also a story about humility. Revaluating your assumptions, revaluating and learning from the data that you generated.”
 Meanwhile, the NIH-funded SCRIPT research team continues to use this machine learning approach to find solutions leading to even better care for critically ill patients, such as giving the right patients the right antibiotic at the right time to reduce the threat of infection with aggressive antibiotic-resistant bacteria. Read more about findings from the SCRIPT Center at Feinberg News Center. Learn how the SCRIPT Center has been supported by investment in next-generation sequencing in Northwestern Medicine Magazine. Meet all of the SCRIPT research team members, contributors, and collaborators here.
Meanwhile, the NIH-funded SCRIPT research team continues to use this machine learning approach to find solutions leading to even better care for critically ill patients, such as giving the right patients the right antibiotic at the right time to reduce the threat of infection with aggressive antibiotic-resistant bacteria. Read more about findings from the SCRIPT Center at Feinberg News Center. Learn how the SCRIPT Center has been supported by investment in next-generation sequencing in Northwestern Medicine Magazine. Meet all of the SCRIPT research team members, contributors, and collaborators here.
Lung Aging Project
The SQLIFTS lung aging project, funded by a National Institutes of Health (NIH) program project grant, has generated novel results with implications for future biomarkers of and interventions for aging and its associated chronic diseases.
Time Ticks Faster for Longer Genes
In an article published in Trends in Genetics and featured on the front page of cell.com, Thomas Stoeger, PhD and collaborators showed that biological aging is associated with decreased expression of longer genes. To describe this phenomenon, found in multiple species including humans, Stoeger and his coauthors introduced the term gene-length-dependent transcription decline (GLTD).
Cell types such as neurons are particularly susceptible to GLTD. One reason is that neurons express long genes, including some of the longest genes known. Another reason is that neurons are postmitotic, so they have more opportunity over their long lives to accumulate DNA damage. These factors predict that GLTD would be seen in Alzheimer's disease—which is what researchers have found. In addition, GLTD is observed under conditions known to accelerate biological aging, such as exposure to tobacco smoke.
This article, shared widely in news releases from both Cell Press and Northwestern University and reported by Medical News Today, expanded on earlier research published in Nature Aging that was featured on Northwestern Now and highlighted by the National Institute on Aging. This discovery was also featured in a Front Matter report published in PNAS.
Looking Ahead to the Future of Aging Research
A new focus on the molecular-level physical processes of aging could provide new insights into old genomic datasets, paving the way for new diagnostic tests or therapeutic targets. As Stoeger told PNAS, "There could be paradigm shifts in interventions, and a new class of biomarkers and interventions that are conceptually different from what others have done in the past."
 Stoeger's publication in Nature Aging was supported by numerous grants awarded by NIH, including the program project grant for the SQLIFTS lung aging project, led by co-author SQLIFTS director Scott Budinger, MD, and for which co-authors SQLIFTS Technology Program director Alexander Misharin, MD, PhD, Health Education Program director Karen Ridge, PhD, and Discovery Program director Navdeep Chandel, PhD, serve as a sub-project and core leaders. This work was also funded by grants awarded by the National Science Foundation, the Department of Defense, and the Department of Veterans Affairs. Services were provided by essential core research facilities funded by both indirect costs and federal grants of their own.
Stoeger's publication in Nature Aging was supported by numerous grants awarded by NIH, including the program project grant for the SQLIFTS lung aging project, led by co-author SQLIFTS director Scott Budinger, MD, and for which co-authors SQLIFTS Technology Program director Alexander Misharin, MD, PhD, Health Education Program director Karen Ridge, PhD, and Discovery Program director Navdeep Chandel, PhD, serve as a sub-project and core leaders. This work was also funded by grants awarded by the National Science Foundation, the Department of Defense, and the Department of Veterans Affairs. Services were provided by essential core research facilities funded by both indirect costs and federal grants of their own.
For his work in the Trends in Genetics article, Stoeger was supported by an NIH K99 award, a research career development grant that supports awardees as they transition from mentored positions into tenure-track or equivalent faculty positions. Stoeger is now an Assistant Professor of Medicine in the Division of Pulmonary and Critical Care with his own laboratory, where he and his research team use a tool they developed to investigate understudied genes related to biological aging that have so far been overlooked in the literature. As Stoeger said in a Nature Technology Feature, “We are in the lucky position to know what we don’t know.”
The link between transcript length and aging is just one of many innovative discoveries to advance the field of aging that will be made by Stoeger in his career with support from federal research funding.
Research Today, Medicine Tomorrow
 Paradigm shifts in the study of aging could have implications not just for aging but for diseases associated with aging. One example is pulmonary fibrosis, which is characterized by progressive and irreversible lung scarring that greatly interferes with lung function. The prognosis is worse than for most cancers, with more than half of patients dying within three years of diagnosis.
Paradigm shifts in the study of aging could have implications not just for aging but for diseases associated with aging. One example is pulmonary fibrosis, which is characterized by progressive and irreversible lung scarring that greatly interferes with lung function. The prognosis is worse than for most cancers, with more than half of patients dying within three years of diagnosis.
At present there are only three drugs approved to treat pulmonary fibrosis, which only slow the progression of the disease. But as the population ages, the number of individuals with pulmonary fibrosis is dramatically increasing, highlighting an urgent need for better treatment options.
Our NIH-funded work at SQLIFTS has identified a suite of molecules that offer hope to patients with pulmonary fibrosis. Some of these new drugs are now in clinical trials, while more are currently under development in the laboratory.
Continuing research with support from NIH will determine which of the molecules being investigated today will become the lifesaving medications of tomorrow.
Aging and Metabolism
SQLIFTS investigators with the lung aging project, funded by a National Institutes of Health (NIH) program project grant, are working toward a deep understanding of the drug metformin and how it could affect metabolism to slow aging.
Probing the Mysteries of a “Wonder Drug”
Derived from a plant (French lilac) used for centuries as an herbal remedy, metformin has been used for nearly 70 years to treat diabetes. But despite its long history and wide use as one of the most prescribed drugs, as well as its known protective effects against cancer and inflammation in cell and animal models, the precise mechanism of action of this “wonder drug” has remained unknown. Now thanks to NIH-funded research at SQLIFTS, we are significantly closer to understanding how metformin works.
 Navdeep Chandel, PhD, director of the SQLIFTS Discovery Program, leads a laboratory dedicated to discovering new biology linked to mitochondria and metabolism that controls physiological responses, disease processes, and aging. He and his group showed that metformin inhibits cancer growth by blocking the function of mitochondrial complex I in cancer cells.
Navdeep Chandel, PhD, director of the SQLIFTS Discovery Program, leads a laboratory dedicated to discovering new biology linked to mitochondria and metabolism that controls physiological responses, disease processes, and aging. He and his group showed that metformin inhibits cancer growth by blocking the function of mitochondrial complex I in cancer cells.
Then researchers including Chandel led by SQLIFTS director and lung aging project leader Scott Budinger, MD found that metformin also targets mitochondrial complex I to decrease lung inflammation induced by air pollution, reducing the risk of heart attacks and strokes. With these and other findings, scientists have hypothesized that mitochondrial complex I could be the key to metformin’s effect on blood sugar.
 In a study recently published in Science Advances, Chandel and his research team provided the first direct evidence in mice that metformin lowers blood glucose levels by inhibiting mitochondrial complex I, thereby discovering the fundamental target and secret sauce of this widely prescribed drug. These findings provide insight into how metformin could work to slow aging through the cascading effects of mitochondrial complex I inhibition.
In a study recently published in Science Advances, Chandel and his research team provided the first direct evidence in mice that metformin lowers blood glucose levels by inhibiting mitochondrial complex I, thereby discovering the fundamental target and secret sauce of this widely prescribed drug. These findings provide insight into how metformin could work to slow aging through the cascading effects of mitochondrial complex I inhibition.
If these results are corroborated and expanded with further research, the future clinical impact could be huge. As Chandel said in a feature in Northwestern Medicine Magazine, “Not only could [metformin] help treat metabolic syndrome—it might ultimately end up that everyone over 70 takes this drug to counteract normal aging deterioration.”
Transforming Our Understanding of Mitochondria
Chandel was awarded the 2023 Lurie Prize in Biomedical Sciences for his contributions as a master of mitochondria who established the organelle’s prominent signaling role beyond its function as the metabolic “powerhouse” of the cell. But after receiving this prestigious accolade, Chandel said his greatest honor was receiving the 2013-2014 Ver Steeg Award for excellence in working with graduate students and postdoctoral scholars, after being nominated by graduate students in his laboratory. A major mission of Chandel’s laboratory is to train the next generation of scientists and physician-scientists in the field of mitochondria and metabolism in a supportive environment. An example of such commitment to training and education is this Science Advances publication.
 First author Colleen Reczek, PhD was supported by the Division of Pulmonary and Critical Care’s T32 training grant, directed by SQLIFTS Health Education Program director and lung regeneration project leader Karen Ridge, PhD. Together, Drs. Ridge and Reczek direct Pulmonary and Critical Care’s Kimberly Querrey Summer Research Program for high school and undergraduate students. (To learn more about both programs, please see the section below on the T32 Lung Science Training Program.) Co-authors Karis D’Alessandro and Zachary Sebo, PhD were also supported by this and other T32 training programs at Northwestern.
First author Colleen Reczek, PhD was supported by the Division of Pulmonary and Critical Care’s T32 training grant, directed by SQLIFTS Health Education Program director and lung regeneration project leader Karen Ridge, PhD. Together, Drs. Ridge and Reczek direct Pulmonary and Critical Care’s Kimberly Querrey Summer Research Program for high school and undergraduate students. (To learn more about both programs, please see the section below on the T32 Lung Science Training Program.) Co-authors Karis D’Alessandro and Zachary Sebo, PhD were also supported by this and other T32 training programs at Northwestern.
Other NIH funding for this study includes the program project grant for the SQLIFTS lung aging project and the program project grant for the lung regeneration project; Chandel serves as a sub-project leader on both. Services were provided by essential core research facilities funded by both indirect costs and federal grants of their own.
Chandel is also well known for his outreach on the science of mitochondria beyond the laboratory, from authoring an introductory textbook, Navigating Metabolism, to featuring in general audience publications such as Quanta magazine, to recording what became one of the top three Breakthroughs podcasts of 2023, How Mitochondria Inform Disease Discoveries.
Thanks to federal funding from NIH, Chandel and his research team at SQLIFTS continue to elucidate the role of mitochondrial signaling in health and disease, and the potential for metformin to restore health in a state of disease such as aging.
T32 Lung Science Training Program
The Northwestern University Lung Science Training Program, funded by a T32 training grant awarded by the National Institutes of Health (NIH), encourages bright, enthusiastic, well-trained, academically oriented MDs and PhDs to pursue careers in pulmonary biology investigation.
Training Tomorrow's Leaders in Science and Medicine
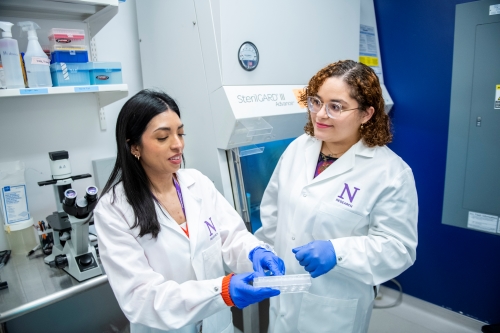 Now in its second decade, the T32 Lung Science Training Program prepares tomorrow’s leaders as they meet the challenges of today by supporting predoctoral and postdoctoral trainees’ research into the pathophysiology of lung disease and translation of these discoveries to the bedside. This federally funded program has trained and supported many physicians now at Canning Thoracic Institute and many more throughout the United States.
Now in its second decade, the T32 Lung Science Training Program prepares tomorrow’s leaders as they meet the challenges of today by supporting predoctoral and postdoctoral trainees’ research into the pathophysiology of lung disease and translation of these discoveries to the bedside. This federally funded program has trained and supported many physicians now at Canning Thoracic Institute and many more throughout the United States.
 The T32 Lung Science Training Program is directed by SQLIFTS Health Education Program director Karen Ridge, PhD, who also leads the SQLIFTS lung regeneration project and is a core leader of both the lung aging project and lung transplantation project, all of which are funded by NIH program project grants to support research conducted in her laboratory. Currently Ridge’s research group includes three PhD candidates in the Driskill Graduate Program in Life Sciences who are supported in their training by this T32 grant.
The T32 Lung Science Training Program is directed by SQLIFTS Health Education Program director Karen Ridge, PhD, who also leads the SQLIFTS lung regeneration project and is a core leader of both the lung aging project and lung transplantation project, all of which are funded by NIH program project grants to support research conducted in her laboratory. Currently Ridge’s research group includes three PhD candidates in the Driskill Graduate Program in Life Sciences who are supported in their training by this T32 grant.
 Ridge is also the executive director of the Kimberly Querrey Summer Research Program, a paid, competitive summer research experience hosted by the Division of Pulmonary and Critical Care for high school and undergraduate students in which T32 trainees serve as mentors. Although this program is generously supported by an endowment from Northwestern University trustees Louis A. Simpson and Kimberly K. Querrey, it relies on a robust network of NIH-funded faculty members who can host interns in their laboratories for the summer.
Ridge is also the executive director of the Kimberly Querrey Summer Research Program, a paid, competitive summer research experience hosted by the Division of Pulmonary and Critical Care for high school and undergraduate students in which T32 trainees serve as mentors. Although this program is generously supported by an endowment from Northwestern University trustees Louis A. Simpson and Kimberly K. Querrey, it relies on a robust network of NIH-funded faculty members who can host interns in their laboratories for the summer.
Thus, the T32 Lung Science Training Program is just one example of the critical importance of federal research funding in educating and training future generations of scientists and physicians. Says Ridge, “Our structured programs prepare scientists and physician-scientists for successful careers in lung health.”
Northwestern's Research Impact: Learn More
We invite you to learn more about the impact of federally funded research at Northwestern University and Feinberg School of Medicine.
Feinberg School of Medicine
Feinberg leads medical research and clinical trials, fueled by federal funding. Our research has a profound impact on our community and beyond. Learn more about the impact of our research.