Presenting Author:
Laura Davidson, M.D.
Principal Investigator:
Ranya Sweis, M.D.
Department:
Medicine
Keywords:
Simulation, Right Heart Catheterization
Location:
Third Floor, Feinberg Pavilion, Northwestern Memorial Hospital
E16 - Education
Mastery Learning of Right Heart Catheterization: Setting the Standard
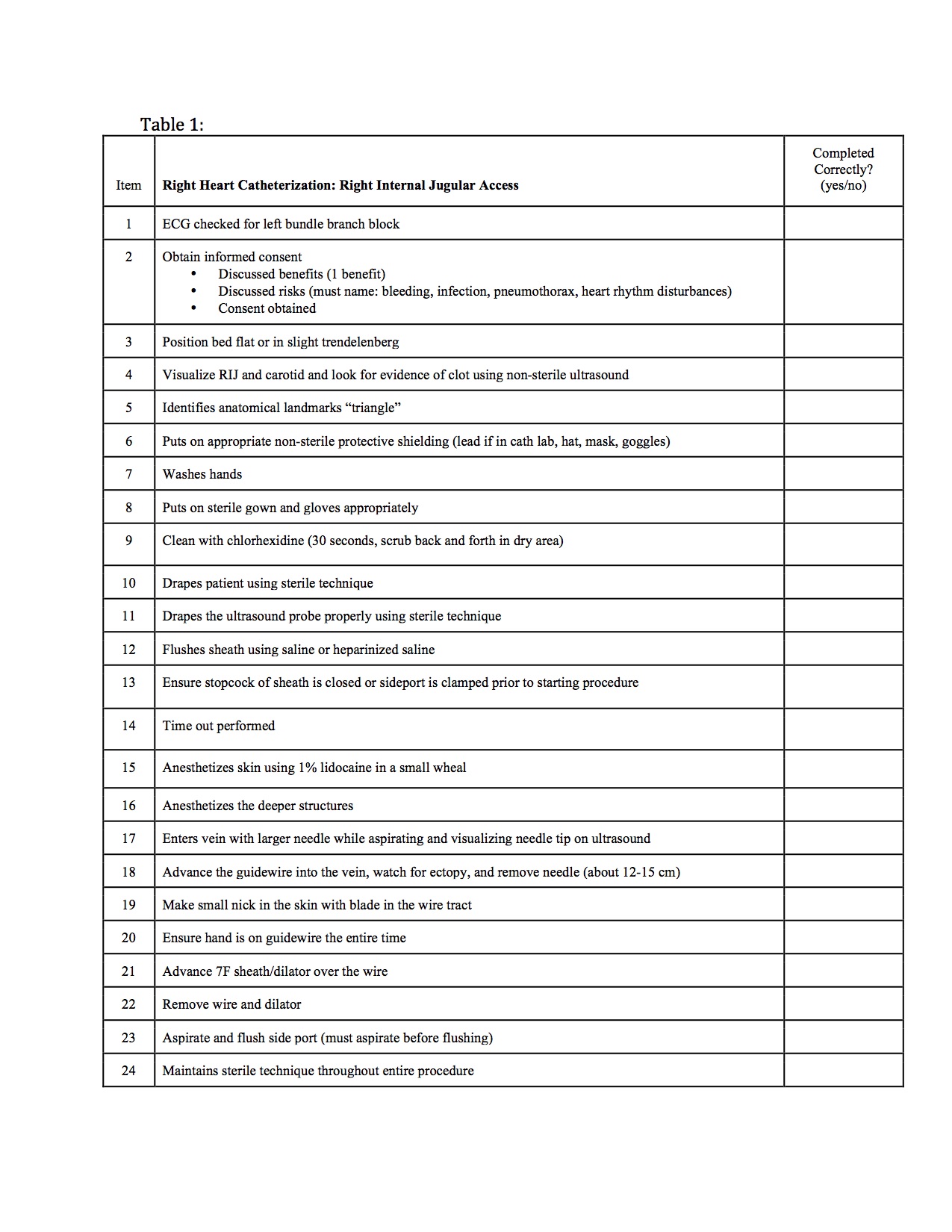
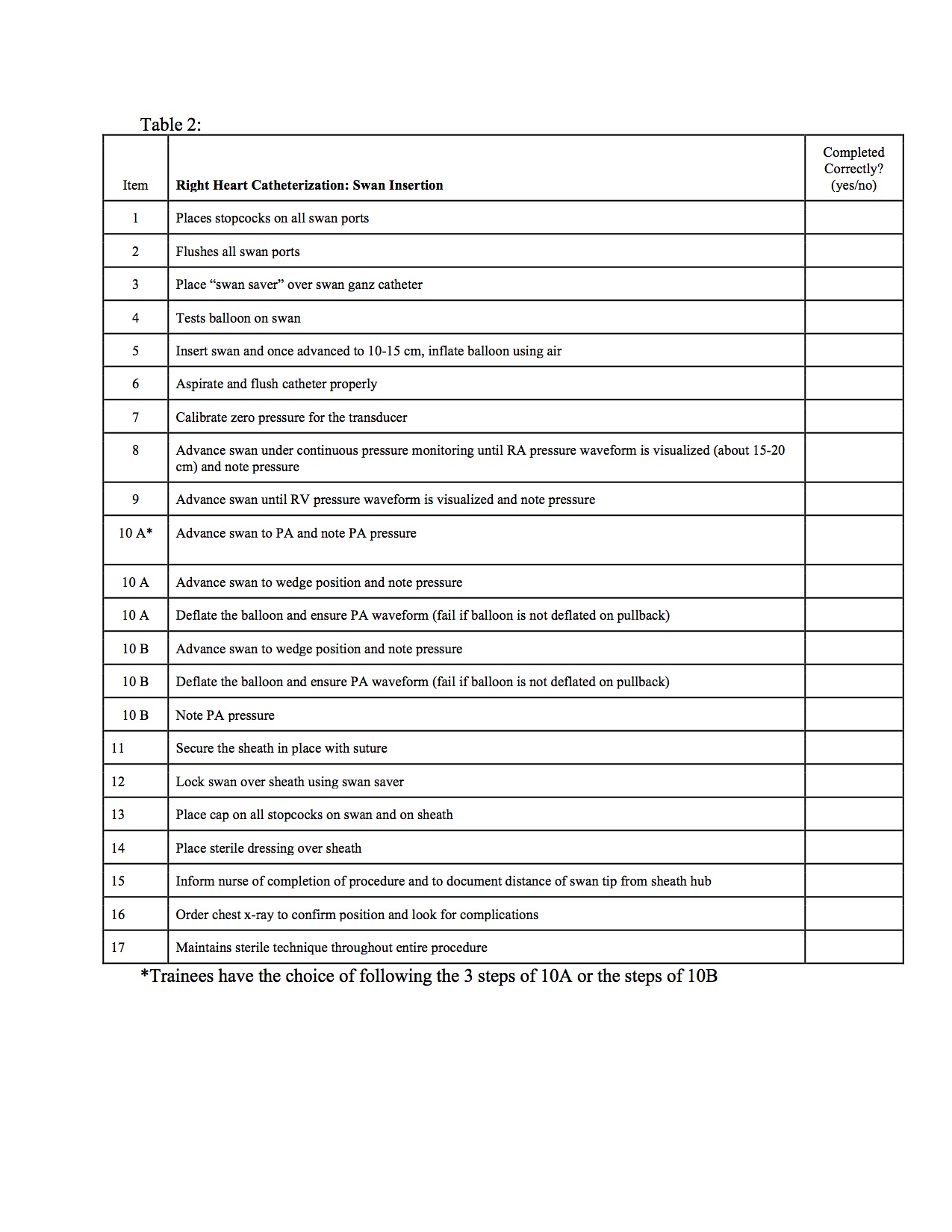
Background: Traditionally, right heart catheterization (RHC) is taught informally at the bedside or in the cardiac catheterization laboratory through observation and practice. As a result, trainees frequently perform RHCs without any formalized training. This can lead to serious complications and patient discomfort. Simulation training, using a mastery-learning model, has been previously shown to reduce iatrogenic injury and improve clinical skills. We aim to develop, implement, and evaluate the efficacy of a RHC simulation curriculum for cardiology fellows, as well as surgery and anesthesia residents to improve trainee competence and clinical outcomes. Here, we present an item-based checklist we developed to evaluate the competence of trainees using a RHC simulator before and after receiving instruction on the simulator. Methods: We developed checklists based on a protocol developed by Western Michigan University that outlined the necessary steps for a successful and safe RHC, which included one checklist for right internal jugular access and a separate checklist for pulmonary artery catheter insertion. We assembled a team of nine experts in RHC, that included interventional cardiology, heart failure, and critical care attendings. Together, these experts edited the checklist and set a minimum passing standard using the previously described Mastery Angoff method. The experts were then asked to use the Patient Safety Method to determine which items on the checklists were critical to be performed correctly in order to ensure patient safety. Results: The final checklists that were developed with the input of our panel of experts are shown (Tables 1,2). After compiling the data obtained from each panel participant, the minimum passing score, as determined by the Mastery Angoff Method, for each skills checklist was found to be 94%. This indicates that each trainee will need to perform 94% of the items on the checklist correctly in order to pass the curriculum and be deemed competent to perform a RHC. This is equivalent to only one permissible incorrect or omitted item on each checklist. Additionally, using the Patient Safety Method, the expert panel collectively agreed that trainees should be able to perform 96% of the items correctly before performing the procedure safely on real patients. Conclusions: Through implementation of previously described methods, we have successfully created RHC procedure checklists and set a minimum passing standard determined by clinical experts for a mastery learning curriculum, which can be utilized in a simulation curriculum that trains inexperienced residents and fellows on the safe and effective performance of RHC. Future studies will utilize this checklist to evaluate trainee performance before and after training on a RHC simulator as well as to evaluate subsequent patient safety outcomes.