Presenting Author:
Principal Investigator:
Department:
Surgery
Keywords:
Cirrhosis Complications MELD Trajectories Predictors
Location:
Ryan Family Atrium, Robert H. Lurie Medical Research Center
C135 - Clinical
Cirrhosis Complications are Poor Predictors of MELD Trajectories
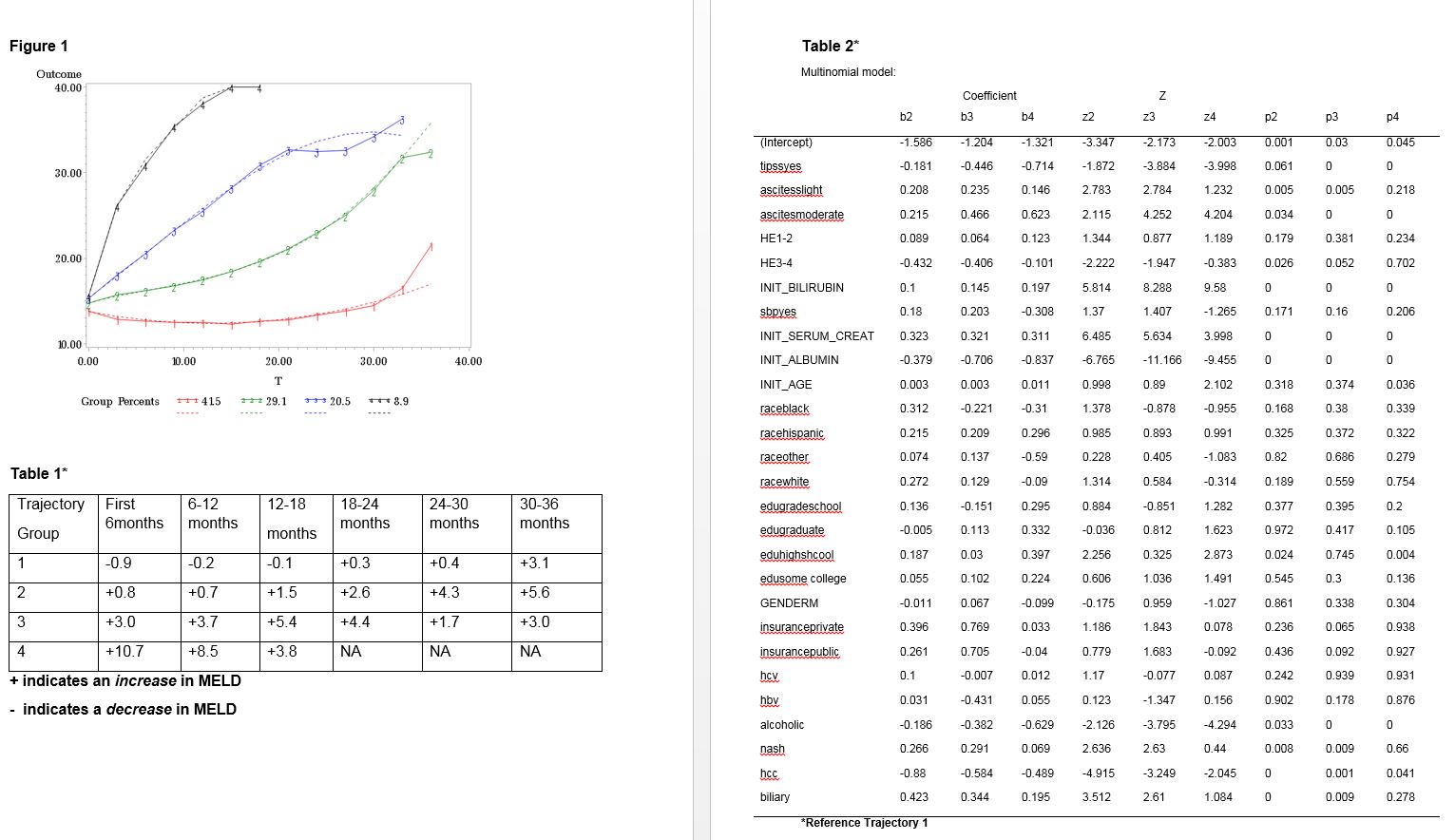
Introduction The ability of the Model of End-Stage Liver Disease (MELD) score to predict mortality for patients with liver cirrhosis is well established. Early prediction at wait-listing for liver transplantation of which patient’s MELD is likely to increase consistently over time would be advantageous, enabling clinicians to encourage timelier intervention given >1500 patients die every year in the US while waiting for a liver transplant. We aimed to identify distinct MELD trajectories for patients on the liver transplant waiting-list and develop a model to predict these trajectories. Methods We used United Network for Organ Sharing (UNOS) data identifying patients placed on the liver transplant waiting-list with MELD at wait-listing of 11-18 from July 2010-June 2015. Patients were followed from wait-listing to either death, liver transplantation or for 3 years. Group based trajectory analysis was employed to identify distinct trajectories of MELD. A competing risk Cox model was used to assess the association of the defined trajectories to either death or transplantation. Multinomial logistic regression was used to identify factors associated with each defined trajectory and to develop a predictive model. Results Data from 8911 patients were used. 5698(64%) were male and 6580 (74%) were white. Mean age was 55 years. The most common reason for wait-listing was Hepatitis C (33%). Median follow up was 0.93 years. 4 distinct trajectories were identified (Group 1-4) Fig1. Table1 describes each trajectory. Compared to Group 1 the HR for death was as follows: Group 2 (HR 1.1 95%CI 0.97-1.3), Group 3 (HR1.6 95%CI 1.4-1.9) and Group 4 (HR 2.68 95% CI 2.2-3.3). Similarly, compared to Group1 the HR for transplantation was as follows: Group 2 (HR 1.1 95%CI 1.02-1.25), Group 3 (HR 2.0 95%CI 1.8-2.2) and Group 4 (HR 2.8 95% CI 2.4-3.2). The multinomial model is provided in Table2. Statistically significant predictors of meld trajectory from this model include ascites, hepatic encephalopathy, serum albumin, alcoholic cirrhosis, non-alcoholic steotohepatitis and hepatocellur carcinoma. The model failed to correctly predict group membership based on distinct trajectory. Group 1 predicted membership n=8042: true membership n=5112. Group 2 predicted membership n=55: true membership n=1801. Group 3 predicted membership n=101: true membership n=1388. Group 4 predicted membership n=22: true membership n=610. Conclusion While complications of cirrhosis are associated with a statistically significant increased risk of MELD progression over time, these complications perform poorly in a predictive model and novel predictors are needed. Decisions regarding timelier intervention for patients waitlisted for liver transplantation will continue to be based largely on clinical acumen and known changes in the MELD score (as opposed to predicted changes) over time.