Presenting Author:
Susan Slattery, M.D.
Principal Investigator:
Susan Slattery, M.D.
Department:
Pediatrics
Keywords:
Neonatal Hypoxic-ischemic Encephalopathy, Length of Stay, Electronic Data Warehouse, Disease Natural History
Location:
Ryan Family Atrium, Robert H. Lurie Medical Research Center
C98 - Clinical
EDW-Derived Features of Neonatal Hypoxic-ischemic Encephalopathy Influencing Length of Stay
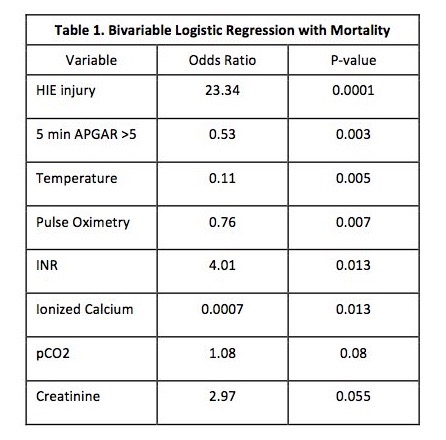
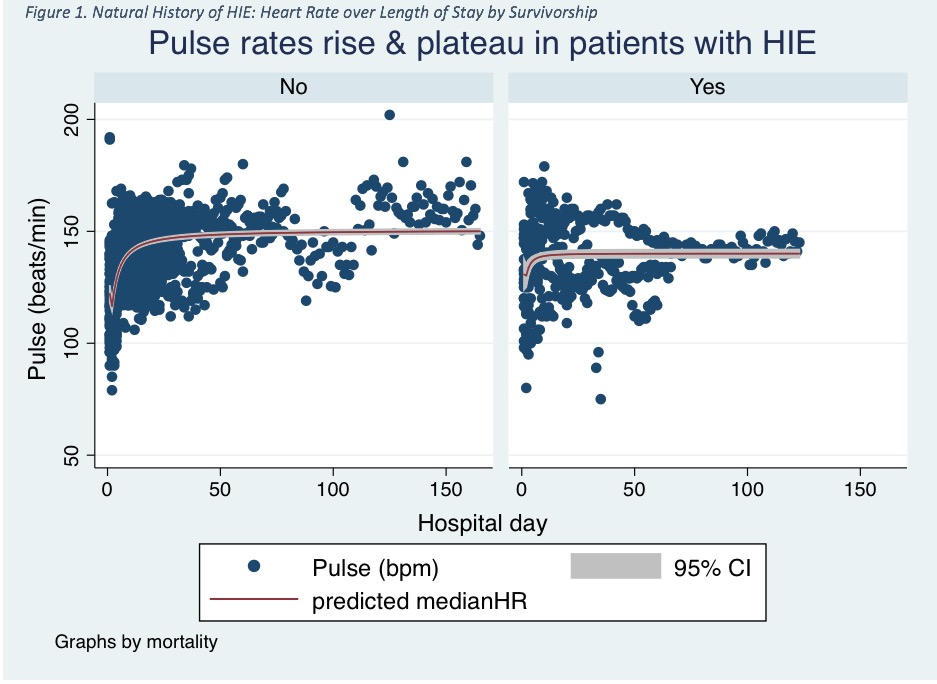
Background: Neonatal hypoxic-ischemic encephalopathy (HIE) is often accompanied by physiologic derangements and organ dysfunction; however, the natural history of these perturbations and their relationship with length of stay (LOS) remains uncertain. Objective: To describe daily markers of physiologic and organ dysfunction in infants with HIE and test their association with LOS in the neonatal intensive care unit. Methods: Eligible subjects were infants with HIE born ≥36 weeks' gestation from 2010-16 and received therapeutic hypothermia. Those with major congenital anomalies were excluded. From our institution’s electronic data warehouse (EDW), we utilized a novel approach linking inpatient clinical markers with records from the Children's Hospitals Neonatal Database. Candidate markers reflected vital signs, pulse oximetry, creatinine, acidosis (pH), ventilation (pCO2), and international normalized ratio (INR). The main outcomes were descriptions of the natural history of these markers, mortality, and time-to-death/discharge stratified by mortality, as appropriate. Multivariable logistic (mortality) and Cox proportional hazards (time to discharge/death) analyses estimated each marker’s independent and a time-varying association with LOS. Covariates included HIE severity, sex, birth weight, seizures, and the 5-minute APGAR score. Results: We identified 66 eligible infants (58% males) and 1671 patient-days; severe HIE (48%) and mortality (32%) were common. Systolic (64±8.7 to 82±5.7 mmHg, p<0.001) and diastolic (40.1±7.7 to 46±6.2 mmHg, p<0.001) blood pressures, heart rate (117±19 to 145±13 beats/min, p<0.001; n=1,203), and pCO2 (0.4 mmHg/day, p=0.001, n=376, Graph 1) each rose, while creatinine levels (1.12 to 0.28 mg/dL, p<0.001) decreased. Multiple variables were independently related to the odds of mortality, and these directly, and indirectly, reflected the severity of illness (Table 1). The median LOS was longer for survivors (8 days [inter-quartile range (IQR) 5-20 d] vs. 24 days [IQR 14-31 d], p<0.001). Among these survivors, over the first 7 days of hospitalization (n=45, 315 days), mean INR levels were independently related to a shorter LOS (hazard ratio (HR) 2.2, 95% confidence Interval (CI) 1.5, 3.2, p<0.001). Among non-survivors, over the hospital stay (n=21, 423 days), rising temperatures (HR = 2.0, 95% CI = 1.2, 3.3, p=0.005) was independently related to shorter survival, while diastolic blood pressure (HR 0.93, 95% CI 0.88, 0.97, p=0.04) was conversely related to survival time. Conclusion: This novel approach capturing discrete patient-level data derived, describing the natural history of an uncommon neonatal disease, and relating their trends with short-term outcomes was successful. Though the relationship with LOS was modest, these results illustrate the use-case of harnessing clinical data toward generalizable information and define the functionalities required to convert the EDW into valued information. (Grant #TL1TR001423)