Presenting Author:
Eddie Blay, M.D.
Principal Investigator:
Anthony Yang, M.D.
Department:
Surgery
Keywords:
thromboembolism, chemoprophylaxis, adherence, refusal
Location:
Ryan Family Atrium, Robert H. Lurie Medical Research Center
C134 - Clinical
Multi-institution Evaluation of Adherence to Comprehensive Postoperative VTE Chemoprophylaxis
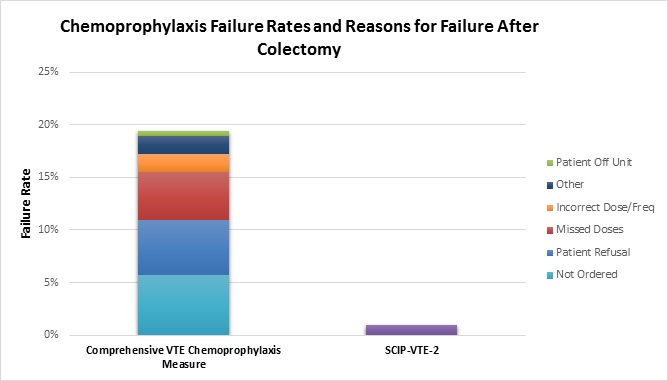
Introduction: Venous thromboembolism (VTE), defined as either a deep venous thrombosis or pulmonary embolism, is a leading cause of preventable postoperative morbidity and mortality. National best practice guidelines recommend chemoprophylaxis, sequential compression devices, and early ambulation for most postoperative surgical patients. Of these, chemoprophylaxis is the most effective in preventing postoperative VTE. Missed doses of chemoprophylaxis are associated with higher VTE incidence. Current measures of appropriate VTE prophylaxis (e.g., SCIP-VTE-2, which measures chemoprophylaxis adherence only in the 24 hours around surgery) are not comprehensive, do not ensure appropriate administration, and cannot identify reasons why failures to provide chemoprophylaxis occur. We examined adherence to a novel comprehensive chemoprophylaxis process measure and patient and hospital-level characteristics associated with measure failure. Methods: Patients ≥ 18 years old who underwent colectomy at hospitals in a statewide surgical collaborative during 2015. Trained data abstractors utilized a novel process measure assessing comprehensive postoperative VTE chemoprophylaxis during a patient’s inpatient hospitalization, including reasons chemoprophylaxis was not given. To pass the measure, patients must have received every prescribed dose of an appropriate VTE chemoprophylaxis drug at the appropriate dose and frequency during their inpatient postoperative hospital stay, unless an accepted exception was documented (e.g., bleeding disorder). Results: Failure to provide defect-free VTE chemoprophylaxis occurred in 511 (19.4%) of 2628 colectomies at 35 hospitals; SCIP-VTE-2 identified failure in only 1% of these cases. Failure reasons included chemoprophylaxis not ordered (29.5%; 151), patient refusal (26.6%; 136), missed dose(s) (23.9%; 122), and incorrect dosage/frequency (8.8%; 45). Teaching hospitals and hospitals without nursing Magnet status more frequently failed to provide defect-free chemoprophylaxis. Patients more frequently experienced chemoprophylaxis failures if younger (≤40 years), had a noncancer diagnosis, or underwent emergent surgery. Patient refusals accounted for half (50.2%) of missed doses and were more frequent in younger patients and at teaching hospitals. Non-teaching hospitals more frequently failed to order any VTE chemoprophylaxis.(all p<0.001) Conclusion: This is the first multi-institution study examining failure patterns in providing comprehensive postoperative VTE chemoprophylaxis. In stark contrast to hospitals’ low rate of failure identified by SCIP-VTE-2 (1%), our measure unmasked chemoprophylaxis failures in 19% of cases. Failure to order postoperative chemoprophylaxis, missed doses, and patient refusals comprise most failures and occur throughout the postoperative period. Thus, hospitals should focus improvement efforts on ensuring patients receive appropriate VTE prophylaxis throughout their entire hospitalization.