Presenting Author:
Maureen Whitsett, M.D.
Principal Investigator:
Lisa VanWagner, M.D.
Department:
Preventive Medicine
Keywords:
NASH, Atrial Fibrillation, Atrial flutter
Location:
Ryan Family Atrium, Robert H. Lurie Medical Research Center
C116 - Clinical
Prevalence and Impact of Atrial Fibrillation among Patients with NASH
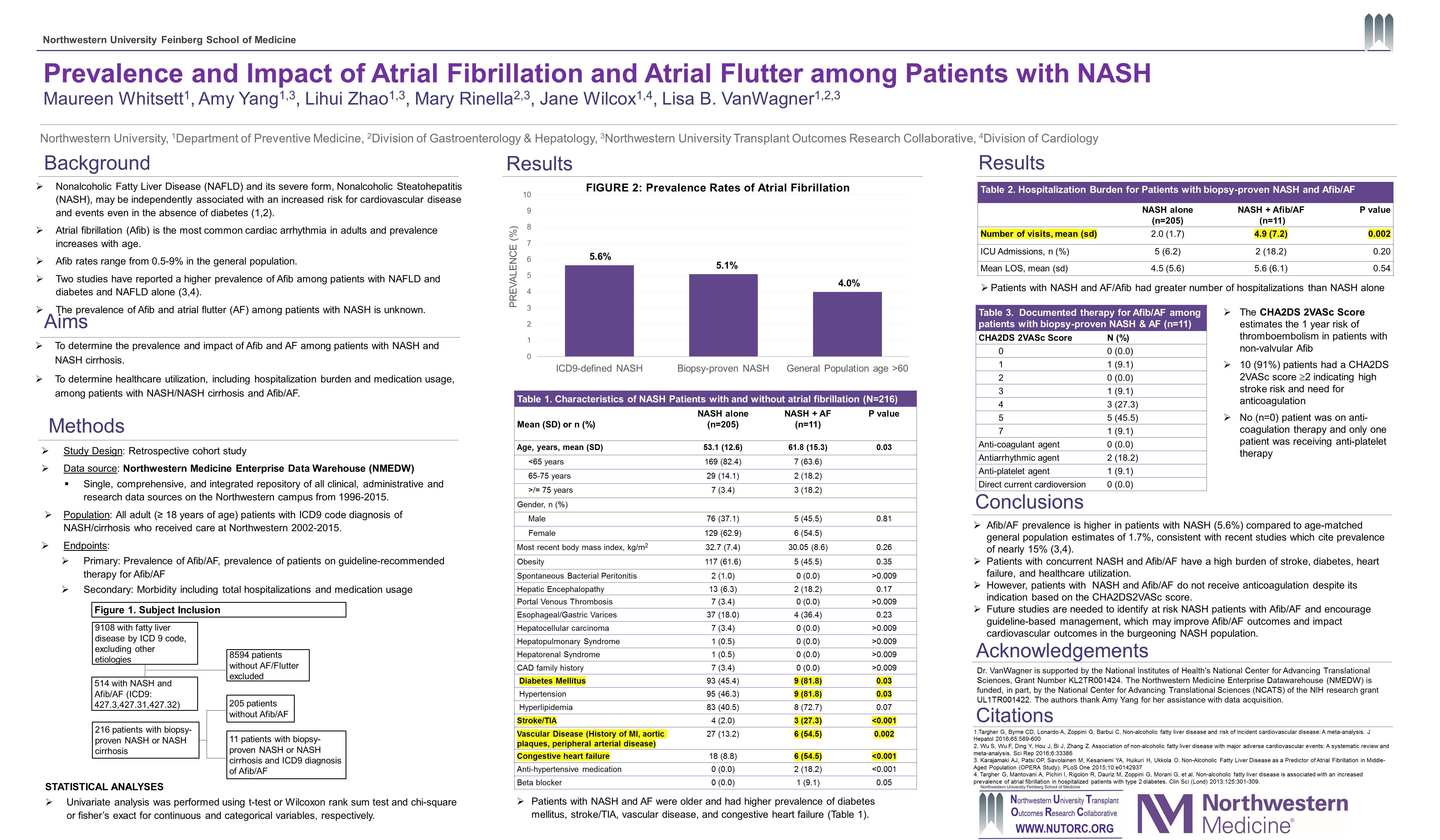
Background: Elevated liver chemistries and ultrasound diagnosed fatty liver are associated with atrial fibrillation (AF) independent of traditional AF risk factors. AF is a potent risk factor for stroke and is associated with poor outcomes after liver transplantation for nonalcoholic steatohepatitis (NASH) cirrhosis. The prevalence of AF in patients with NASH or NASH cirrhosis is unknown. Purpose: To assess the prevalence and impact of AF on healthcare utilization in patients with NASH or NASH cirrhosis. Methods: Patients with biopsy-proven NASH or NASH cirrhosis were identified using ICD9 billing codes from a tertiary care center Electronic Database from 2002-2015. NASH/cirrhosis was confirmed though independent review of liver biopsy reports at our center. ICD9 codes identified the presence of comorbidities and AF prevalence. T-test, Chi-square or Fisher exact tests were used to compare medication usage and comorbidities, as well as hospitalization and length of stay between patients with NASH and AF versus patients with NASH without AF. Results: Of 9108 patients with an ICD9 diagnosis of NASH/cirrhosis, 514 (5.6%) patients had a coexisting diagnosis of AF, and 216 (2.37%) had biopsy-proven NASH/cirrhosis. Mean age of biopsy-proven NASH/cirrhosis patients was 53.05 ± 12.58 years and 37.1% were male. The prevalence of AF was 5.09% in biopsy-proven NASH/cirrhosis. Four patients with biopsy-proven NASH and AF had cirrhosis. Patients with NASH/cirrhosis and AF were older (62.7 vs. 53.1 years) and had a higher prevalence of hypertension (81.8% vs. 46.3% p=0.029), diabetes mellitus (81.8% vs. 45.4%, p=0.027), heart failure (54.5% vs. 8.8%, p<0.001) and cerebrovascular (27.3% vs. 2%, p<0.001), or vascular disease (54.5% vs. 13.2%, p=0.002), compared to those without AF. Among biopsy-proven NASH/cirrhosis patients, 10 (91%) had a CHA2DS2VASc score 2 indicating high stroke risk and need for anticoagulation. No patients were on anticoagulation and only 1 patient was on an anti-platelet agent. No patients received cardioversion or ablation. Patients with NASH and AF had more hospital visits (4.91 vs. 1.95, p=0.002) and statistically insignificant longer hospital stays compared to those without AF (5.64 vs. 4.51 days, p=0.535). Conclusion: AF prevalence is higher in patients with NASH and NASH cirrhosis compared to general population estimates of 1.7%. Patients with concurrent NASH/cirrhosis and AF have a high burden of stroke, heart failure, diabetes, and healthcare utilization. However, NASH/AF patients do not receive anticoagulation despite its indication based on the CHA2DS2VASc score. Future studies are needed to identify at risk NASH patients with AF and encourage guideline-based management. This may improve AF outcomes and impact cardiovascular outcomes in the burgeoning NASH population.