Presenting Author:
Lindsay Pool, Ph.D.
Principal Investigator:
Mercedes Carnethon, Ph.D.
Department:
Preventive Medicine
Keywords:
Affordable Care Act; cardiovascular disease; risk factors; prevention; screening; surveillance; socioeconomic status; insurance
Location:
Third Floor, Feinberg Pavilion, Northwestern Memorial Hospital
PH41 - Public Health & Social Sciences
Cardiovascular Preventive Service Use Trends During Affordable Care Act Implementation
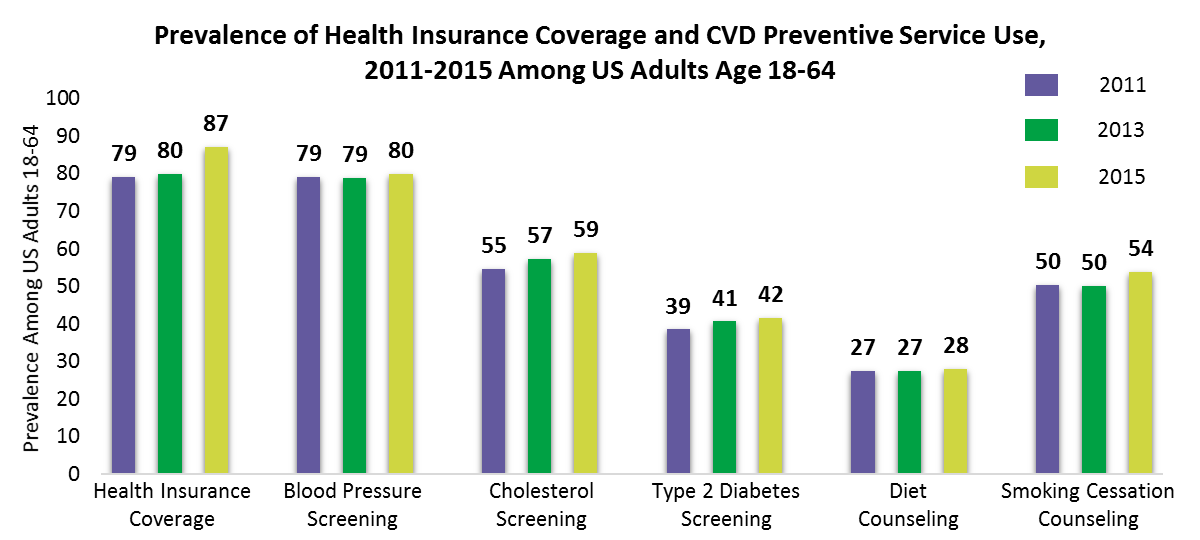
Background: The Affordable Care Act (ACA), signed into law in 2010, was incrementally implemented by a series of reforms including an expansion of health insurance coverage and preventive services coverage without co-pay. It is not known whether cardiovascular disease (CVD) preventive services have increased as a result of enhanced healthcare access. Hypothesis: We hypothesized that CVD risk factor screening and counseling would increase among US adults under age 65 during the period of ACA implementation, 2011-2015. Methods: The National Health Interview Survey is a telephone survey of a random sample of the US civilian noninstitutionalized population. Adult respondents from survey years 2011, 2013, and 2015 were asked whether, in the past year, they had a screening test for blood pressure, cholesterol, and diabetes, and counseling about diet and smoking cessation from a health professional. We included adults under age 65 only (n=78,231), due to near universal health coverage in older adults prior to the ACA. We calculated prevalence differences (PD) from 2011 to 2015 for each preventive service using weighted Poisson regression with robust variance. We further examined whether prevalence changes were similar during 2011-2013 as compared to 2013-2015, as well as by household income levels (relative to the federal poverty level). Results: Health insurance coverage increased from 2011-2015, primarily among lower income groups. There were significant increases in the prevalence of blood pressure, cholesterol, and diabetes screenings, and smoking cessation counseling during the implementation period (Figure 1). Individuals in the highest income group experienced significant increases in cholesterol and diabetes screenings from 2011-2013, when preventive services coverage commenced for existing health insurance plans. Individuals not in the highest income group experienced significant increases in blood pressure and diabetes screenings, and smoking cessation counseling during 2013-2015, concomitant with health insurance coverage increases. Lower income individuals experienced increases in cholesterol screening during both 2011-2013 and 2013-2015. Conclusions: CVD risk factor screening and counseling increased during ACA implementation. Higher income individuals had high prevalence of health care coverage prior to the ACA, but may have benefited from preventive services coverage without co-pay, with improved prevalence of cholesterol and diabetes screening. Lower income individuals had significant gains in health care coverage, along with improved prevalence of screening and counseling. Outreach is needed to ensure newly insured persons are aware of covered CVD preventive services, as socioeconomic disparities in overall rates of CVD screening and counseling continue to persist.