Presenting Author:
Amandeep Jutla, M.D.
Principal Investigator:
Amandeep Jutla, M.D.
Department:
Psychiatry and Behavioral Sciences
Keywords:
antidepressants, psychopharmacology, autism spectrum disorder, depression, epidemiology, preventive healthcare
Location:
Ryan Family Atrium, Robert H. Lurie Medical Research Center
C122 - Clinical Women's Health Research
Is prenatal antidepressant exposure associated with autism spectrum disorder?
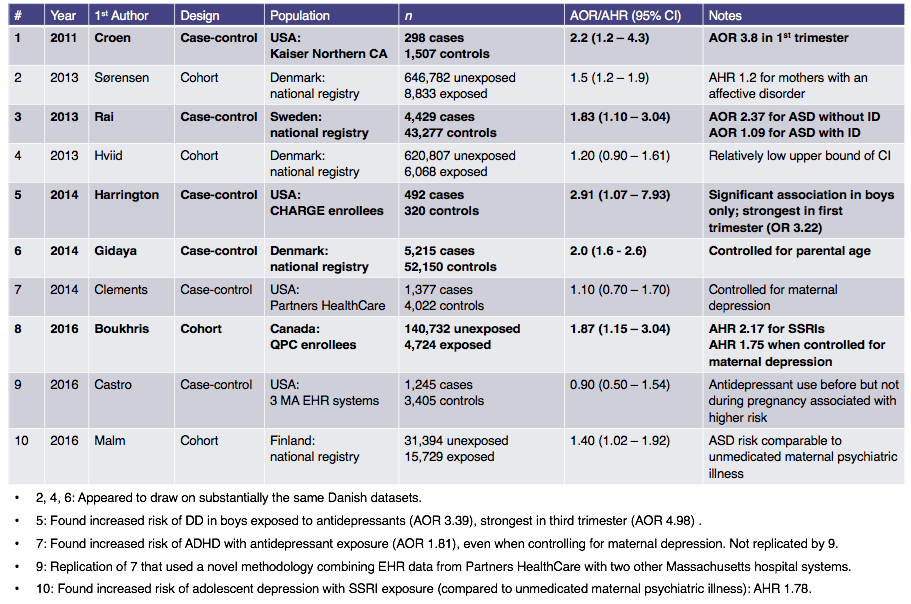
Background: Serotonin has an important role in the human central nervous system. As a trophic factor during development, it may influence the ability to manipulate and process information by directing the differentiation and microstructural organization of the cortex, and may also influence the ability to apprehend sensory stimuli via its role in the development of the somatosensory cortex. Furthermore, as a neurotransmitter, serotonin may, either alone or in conjunction with the neuropeptide oxytocin, have an effect on the modulation of social behavior. Autism spectrum disorder (ASD) is notably characterized by abnormalities in these same three domains of information processing, the interpretation of sensory stimuli, and social behavior. Furthermore, ASD has been repeatedly associated with abnormalities of the serotonin system: peripheral hyperserotonemia, for example, may occur in 25 to 41% of individuals with ASD. The most commonly prescribed antidepressants are selective serotonin reuptake inhibitors (SSRIs), which alter extracellular serotonin levels in the brain and are known to cross the placenta. Therefore, in principle, there is a plausible mechanism of action by which maternal use of SSRI antidepressants could be an ASD risk factor for the developing fetus. Is there evidence to suggest that such a risk truly exists? Methods: A review of the extant literature identified six case-control studies and four cohort studies that specifically examined a potential association between prenatal antidepressant exposure and ASD. Methodologies, inclusion and exclusion criteria, adjusted covariates, and results were qualitatively compared. Results: 4 of 6 case-control studies and 1 of 4 cohort studies found a statistically significant increase in ASD risk with maternal antidepressant use. If such an increase exists, it may be highest in the first trimester. Importantly, major potential confounders (including maternal psychiatric illness, advanced maternal age, and advanced paternal age) were not controlled for in all studies, and even in studies where an association was found, absolute risk was modest. Conclusions: Data are equivocal regarding whether prenatal antidepressant exposure is an ASD risk factor: existing studies are heterogeneous in design and in terms of adjusted covariates, and have yielded conflicting results. Any possible risk would have to be weighed against the risks of untreated maternal depression. More research in this area is needed so that clinicians and patients can make informed decisions regarding treatment of depression during pregnancy.