Presenting Author:
Danica Aniciete, M.S.
Principal Investigator:
Kelly Michelson, M.D.
Department:
Pediatrics
Keywords:
Communication, Decision Making, Navigator, Pediatric Intensive Care Unit, Support.
Location:
Ryan Family Atrium, Robert H. Lurie Medical Research Center
C91 - Clinical
Improving Communication in the PICU: PICU Supports Pilot Study
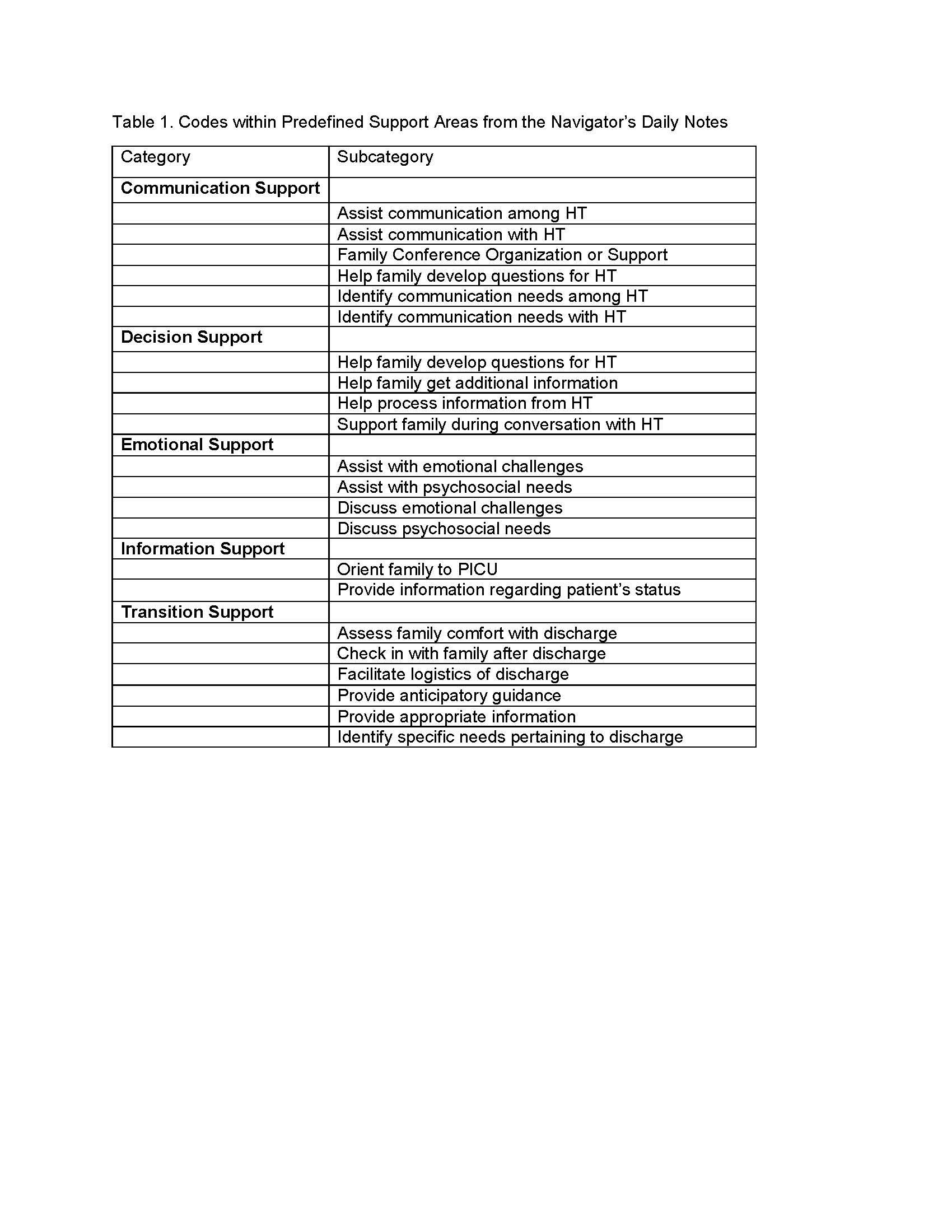
Background/Objective: The use of navigators is new to the pediatric intensive care unit (PICU). We pilot tested a navigator-based intervention called PICU Supports. PICU Supports seeks to provide emotional, communication, decision making, information, and transition support. PICU Supports involves weekday interactions between the navigator and parents and the healthcare team (HT) as well as navigator guided use of ancillary tools (such as a handbook and parent diary). The navigator focuses on individual needs/desires as determined by the parent. Here we describe the support provided by the navigator based on notes taken by the navigator following interactions with parents and the HT. Methods: Parents of PICU patients were eligible if they spoke English or Spanish, their hospitalized child was <18 years old, had a projected PICU length of stay > 24 hours, and if the PICU attending gave permission. The navigator met with parents on weekdays until PICU discharge with one “check-in” after PICU discharge. The navigator kept notes about discussions with parents and HT members. Notes were categorized into predefined support areas: emotional (psychosocial issues); communication (parents’ perception of communication in the PICU); decision making (identifying issues and supporting parents with decision making); transition (preparing parents for discharge or transition after the PICU), and information (providing relevant information). Using content analysis we qualitatively analyzed the navigator’s notes and developed theme-based codes for each support area. We present frequencies of code occurrences using descriptive statistics. Results: We enrolled 38 parents of 35 PICU patients at Lurie Children’s Hospital between November 2014 and April 2015. 73% (n=28) of enrolled parents were mothers. 39% (n=15) of parents identified as White, 24% (n=9) Black, 3% (n=1) Alaskan Native/American Indian, 3% (n=1) Native Hawaiian / Pacific Islander, 3% (n=1) Asian, and 28% (n=11) “Other”. 29% (n=11) of parents identified as Hispanic. Parents were on average 33.4 years old (median 33, range 21-49). Patients were on average 4.4 years old (median 2.3, range .07-17.6). Patients had an average Pediatric Index of Mortality 2 (PIM2) score of 2.63 (median 1.1, range 0.2-12.7) and an average length of stay of 10.6 days (median 1, range 1-32 days). There were 457 excerpts recorded for the pre-defined support areas distributed as follows: emotional (n=194, 42.5%); communication (n=122, 26.7%); decision (n=35, 7.7%); transition (n=71, 15.5%); and information (n=35, 7.7%). Table 1 describes the codes created within each support area. Conclusions: The prominent focus of the navigator’s interactions with parents and the HT involved providing communication and emotional support. Future work will provide more detail about the issues within each support category and consider the relationship between identified challenges and parent outcomes.