Presenting Author:
Alexandra Haugh, B.A.
Principal Investigator:
Pedram Gerami, M.D.
Department:
Dermatology
Keywords:
melanoma, hereditary cancer syndromes, genetics
Location:
Ryan Family Atrium, Robert H. Lurie Medical Research Center
C9 - Clinical
The BAP1 Cancer Syndrome: A Case Series and Literature Review
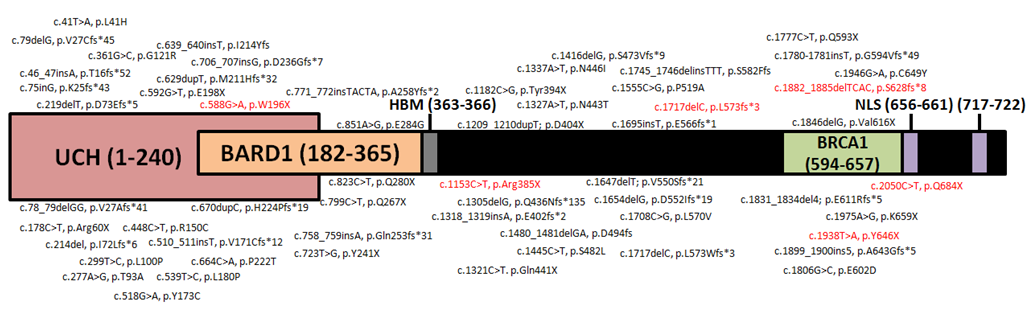
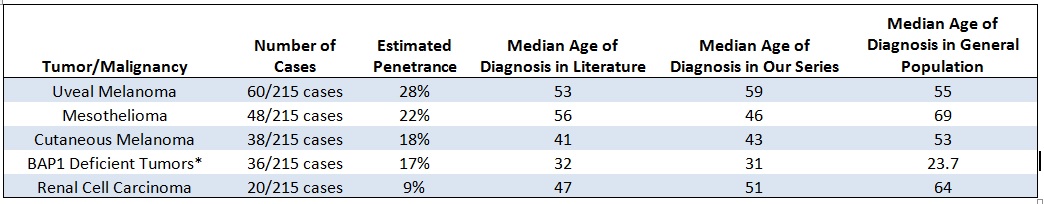
Importance: Patients with germline mutations in BAP1 may develop several flesh-colored BAP1-deficient tumors (BDTs). These tumors generally develop earlier than other associated tumors, highlighting an important role for dermatologists in identifying and screening patients with a history suggestive of a germline mutation. Objective: To describe 8 new families with germline mutations in BAP1 and provide a comprehensive review of reported cases. Design: Patients were identified in a clinical setting from June –December 2016 and a literature review was performed using PubMed. Setting: Patients were identified in outpatient dermatology clinics. Participants: Ten patients were identified through clinical screening and an additional 205 patients were identified through literature review. Methods: Mutations were identified through Next Generation Sequencing (NGS). DNA was extracted from fibroblasts cultured from a patient with an intronic variant to determine the impact of the mutation on the coding sequence. Outcomes and Measures: All 215 patients were assessed for personal /family history of malignancy and genotype. These findings were compiled and assessed for any association between genotype and phenotype. Results: Uveal melanoma is the most prevalent malignancy among BAP1 mutation carriers (28%) followed by mesothelioma (22%), cutaneous melanoma (18%), and renal cell carcinoma (9%). Nine of the ten patients presented in our study and 75% of all included patients who underwent total body skin examinations were found to have BDTs on clinical exam. A total of 71 unique mutations in BAP1 were identified, a majority of which were expected to lead to protein truncation. Conclusions and Relevance: Our results indicate that germline mutations in both coding and non-coding regions throughout the BAP1 gene can impair protein function, leading to an increased risk for several associated malignancies. Four of the 8 probands we present had no history of BAP1 associated malignancies and were assessed for germline mutations when found to have BDTs on dermatologic exam between the ages of 10-33. Dermatologists can identify patients with the BAP1 cancer syndrome by assessing personal and family cancer history in patients found to have BDTs on routine clinical exam.