Presenting Author:
Elizabeth Addington, Ph.D.
Principal Investigator:
Judith Moskowitz, Ph.D.
Department:
Medical Social Sciences
Keywords:
Positive affect, HIV, opioids, headaches, pain, non-pharmacologic pain management
Location:
Third Floor, Feinberg Pavilion, Northwestern Memorial Hospital
PH12 - Public Health & Social Sciences
Positive Affect Skills Improve Pain Management in People with HIV
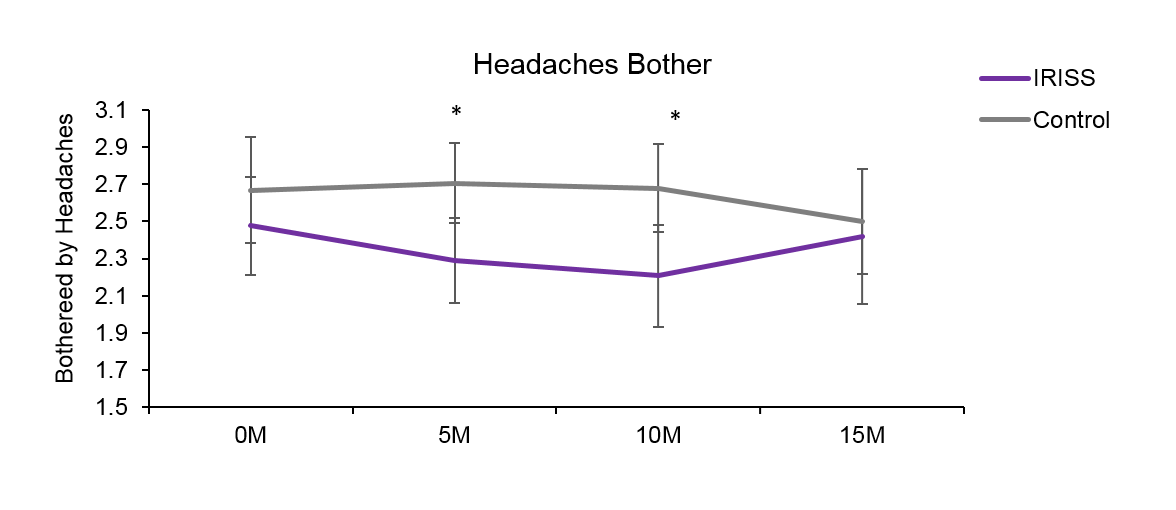
BACKGROUND: Chronic pain is prevalent in the US population and among people with HIV. It is associated with negative psychosocial and medical/economic outcomes such as depression, poorer quality of life, and increased healthcare utilization. Overuse of opioids has resulted in a public health crisis. Paradoxically, opioids can exacerbate pain in people with HIV. Trials of non-opioid pharmaceuticals tend to be biased and lack scientific rigor, and trials of behavioral interventions are scant. The need for safe and effective pain management strategies for people with HIV therefore remains critical. Positive affect is associated with a wide range of benefits in physical and mental health. This study therefore used a series of secondary analyses to examine pain-related outcomes in IRISS, a randomized controlled trial of a behavioral intervention to increase positive affect in people newly diagnosed with HIV. METHOD: Participants (n=159, 92% male, mean age = 36) were randomized to receive 5 weeks of instruction in positive affect skills (i.e., noticing and capitalizing on positive events, gratitude, mindfulness, positive reappraisal, personal strengths, goal attainment, acts of kindness) or a time- and attention-matched control. In measures administered at baseline, post-intervention (5 months post-diagnosis), and 10 and 15 months post-diagnosis, participants reported whether they experienced headaches in the past 30 days, how much their headaches bothered them, and whether they had used opioids. Using intent-to-treat analyses, longitudinal growth models were examined for differential patterns of change over time in the intervention vs. control group. RESULTS: At baseline, prevalence of headaches, levels of headache-related bother, and rates of opioid use were equivalent (p>.05) between groups. Among those with headaches (41% intervention, 30% control at baseline), generalized estimating equations revealed a significant quadratic effect (p=.05) of the intervention on headache-related bother over time. Effect sizes for between group differences in change from baseline were d=-.27 at post-intervention and d=-.34 at 10 month follow-up. By 15 months, headache-related bother began to converge, such that the groups did not significantly differ at the final assessment. In the intervention group, opioid use remained fairly stable over time (17%, 16%, 15%, 15%), while it increased over time in the control condition (18%, 22%, 26%, 30%). Although the group difference in change from baseline did not reach statistical significance (p=.076), the effect size for the between-group difference in change from baseline to the 15-month assessment was d=-.43. CONCLUSIONS: This study provides initial support for the efficacy of the IRISS intervention to improve pain management in people with HIV. If replicated in future trials designed to target pain outcomes, positive affect skills have the potential to significantly improve public health by decreasing pain and opioid use.