Presenting Author:
Andrew Schneider, M.D.
Principal Investigator:
Erin Hsu, Ph.D.
Department:
Orthopaedic Surgery
Keywords:
Hyperelastic bone, spinal fusion, hydroxyapatite, demineralized bone matrix, ceramic, scaffold
Location:
Third Floor, Feinberg Pavilion, Northwestern Memorial Hospital
B124 - Basic Science
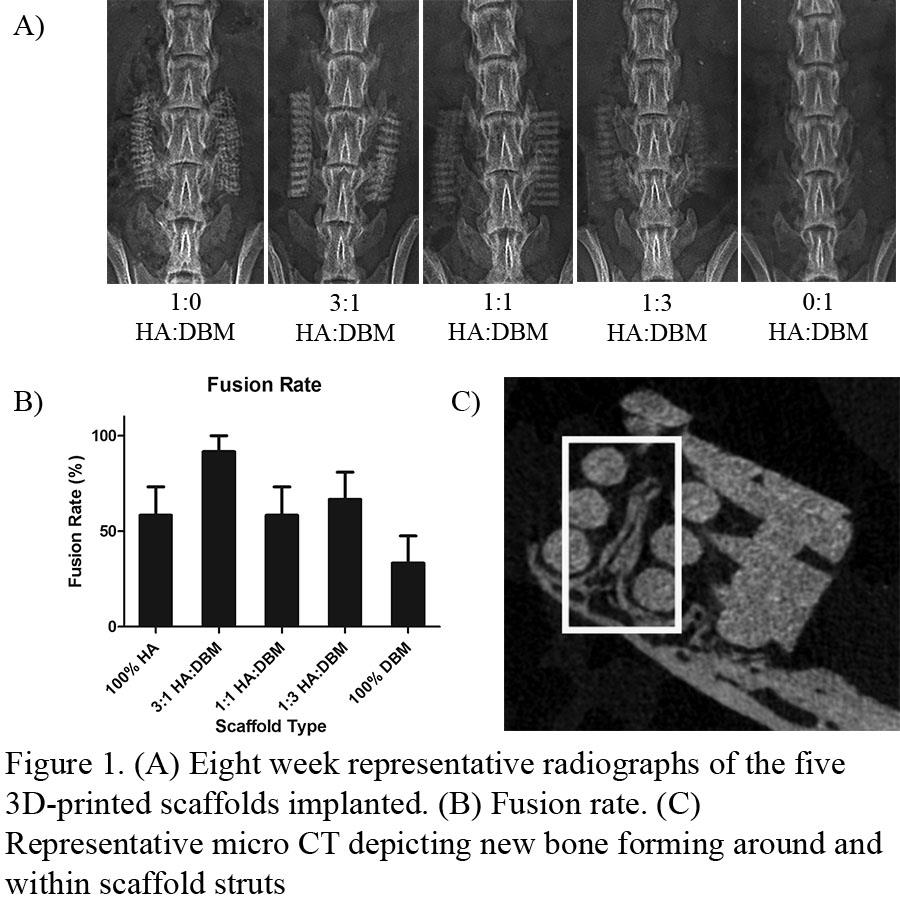
Ceramic-Demineralized Bone Matrix Ink for 3D-printing Scaffolds for Spinal Fusion
INTRODUCTION: Pseudarthrosis occurs in 10-15% of patients who undergo spine fusion. The development of an efficacious and safe bone graft substitute (BGS) is a major research focus. Recombinant human bone morphogenetic protein-2 (rhBMP-2) is a biologic BGS that elicits high fusion rates but is associated with serious adverse effects. Both DBM and synthetic ceramics have improved safety profiles over rhBMP-2, but alone have insufficient osteoinductivity, low structural strength and/or poor handling properties. We have developed a unique 3D-printable biomaterial ink consisting of various hydroxyapatite (HA)-demineralized bone matrix (DBM) compositions to 3D-print Hyperelastic “Bone” composite (HBC) scaffolds. We evaluated the capacity of these HBC scaffolds to promote bone regeneration and spine fusion in a rat posterolateral spine fusion (PLF) model. METHODS: After obtaining IACUC approval, 60 Sprague-Dawley rats underwent a posterolateral spine fusion at L4-L5 with placement of one of five Hyperelastic “Bone” scaffolds. Each scaffold consisted of 30 vol.% PLGA, which served as an elastomer. The remaining 70 vol.% was composed of varying ratios of HA and DBM particles. Treatment groups were as follows: (1) 1:0 HA:DBM; (2) 3:1 HA to DBM; (3) 1:1 HA to DBM; (4) 1:3 HA to DBM; or (5) 0:1 HA:DBM [Figure 1A]. At 8 weeks postoperative, spines were evaluated for bone formation and successful fusion using plain radiographs, manual palpation for motion between segments, and synchrotron microCT imaging. Fusion was assessed via manual palpation by 3 blinded investigators using an established scoring system: 0=no fusion, 1=unilateral bridging and lack of motion between segments, and 2=bilateral bridging and lack of motion. Spines with an average score 1.0 were considered successfully fused. RESULTS: In the animals treated with the 3:1 HA:DBM composite, 11/12 (92%) achieved successful fusion. This was greater than the 7/12 (58%) seen in both the 1:1 HA:DBM and 1:0 HA:DBM groups, the 8/12 (67%) rate seen in the 1:3 HA:DBM group, and the 5/12 (42%) in the 0:1 HA:DBM alone group [Figure 1B]. MicroCT imaging showed new bone formation integrating within the implanted scaffold [Figure 1C]. DISCUSSION: This study evaluated the use of novel HA-DBM biomaterial inks to 3D-print hyperelastic bone composite (HBC) scaffolds containing varying ratios of bioactive components. Both the HA and DBM components are osteoconductive and osteoinductive, and all variations of composites had advantageous handling properties over many of the currently available ceramic-based bone graft substitutes. Fusion scoring suggests that a ratio of 3 parts HA to 1 part DBM may represent the most potent iteration for spine fusion in the rat PLF model. Continued improvements and modifications to the 3D-printed scaffold architecture (e.g. pore size, strut configuration, etc.) may further improve the bone regenerative capacity of the HBC.