Presenting Author:
Nina Ayala, M.D.
Principal Investigator:
Shohreh Shahabi, M.D.
Department:
Obstetrics and Gynecology
Keywords:
Peripartum hysterectomy, obesity,
Location:
Ryan Family Atrium, Robert H. Lurie Medical Research Center
C70 - Clinical Women's Health Research
Increased Morbidity Associated with Peripartum Hysterectomy in Obese Patients
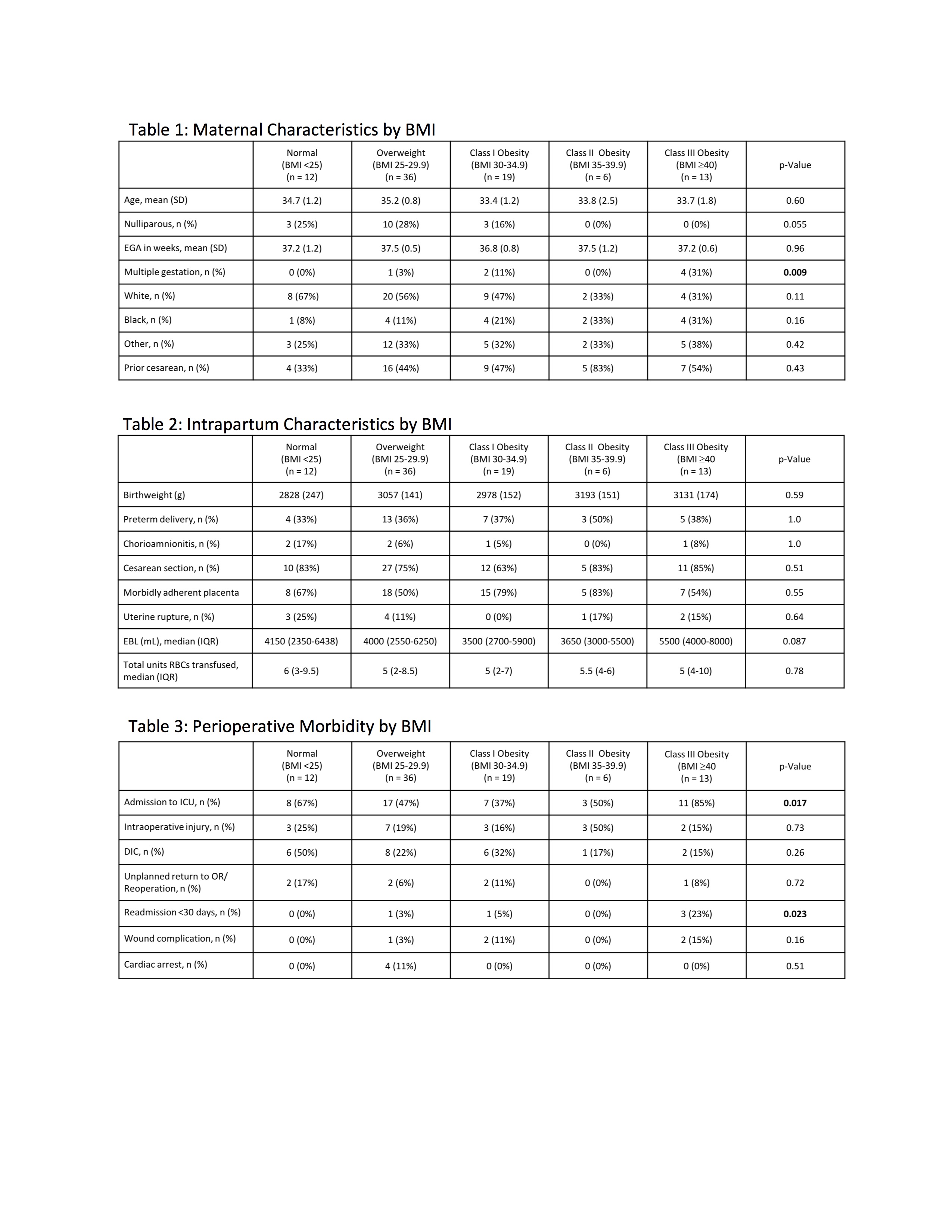
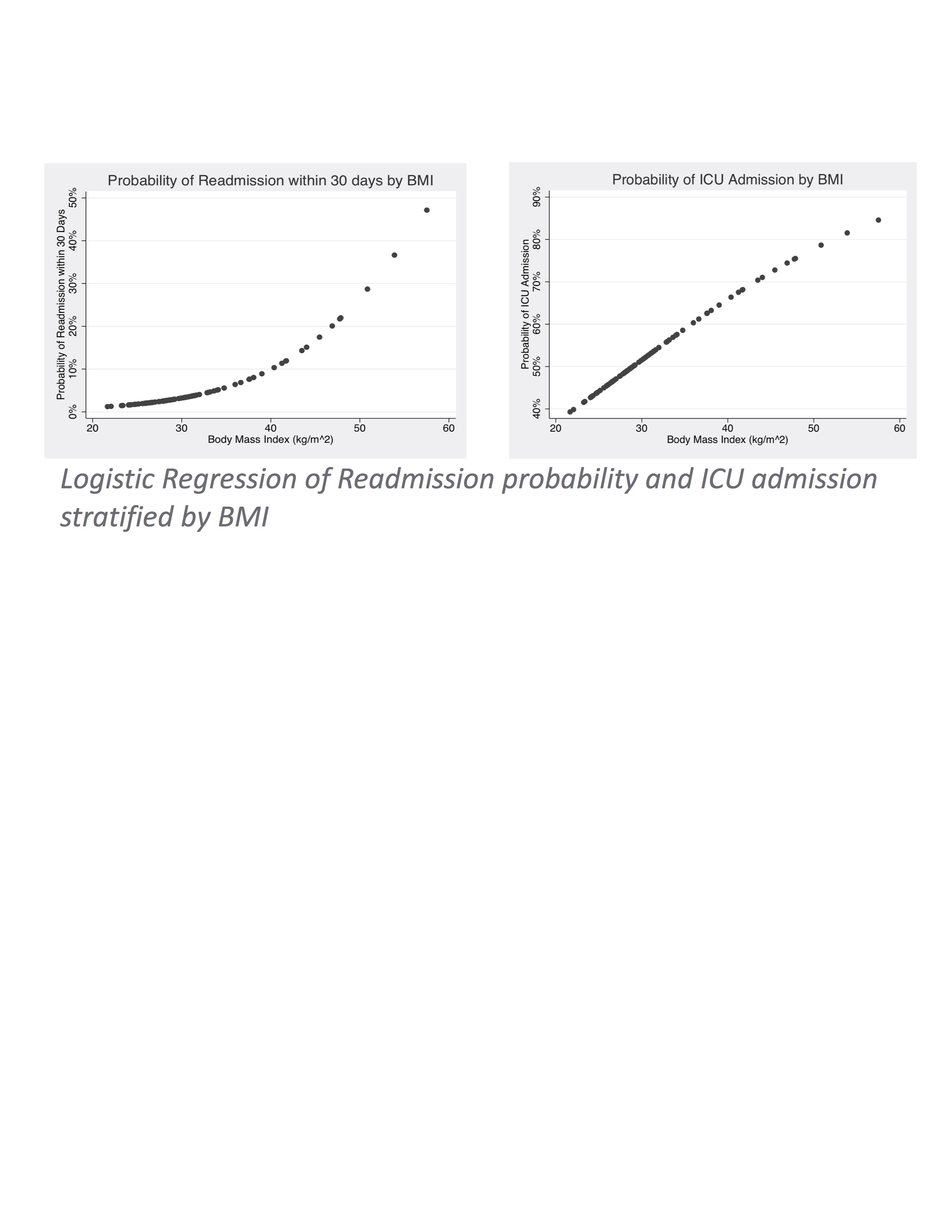
Objective: Maternal obesity is an independent risk factor for morbidity in pregnancy and at the time of cesarean section. We hypothesized that obesity would also be an independent risk factor for morbidity at the time of peripartum hysterectomy. Study Design: This is a retrospective chart review of all peripartum hysterectomies performed at NMH from 1/2010-12/2014. Demographic information, labor and delivery outcomes, estimated blood loss, blood product resuscitation as well as associated complications, hospital readmissions at <30 days and mortality data were collected. Results: A total of 86 cases were reviewed, and average BMI in this cohort was 31.6 with 38 patients (44.2%) meeting criteria for obesity (BMI >30) and 13 (15%) for Class III obesity (BMI >40). Patients with Class III obesity had increased rates of ICU admission with 84.6% of pts admitted to ICU having BMI >40 compared to 47.9% in pts with BMI <40 (p = 0.017). In the multivariable analysis, the relationship between Class III obesity and ICU admission remained despite controlling for EBL, development of DIC and product resuscitation with >4U RBCs. Patients requiring readmission at <30 days had higher BMI than those that did not (40.6 vs 31.0, p= 0.0051) with a trend toward obese patients with operative injuries representing a proportionally higher readmitted group. We estimated the probability of readmission stratified by BMI and the probability curve was exponential, with an upward inflection point around BMI=38, and probabilities exceeding 10% for those with a BMI > 40. Conclusion: Our study demonstrates Class III obesity is an independent risk factor for increased morbidity at the time of peripartum hysterectomy including need for ICU admission and <30 day readmission rates. As peripartum hysterectomy is an increasingly common obstetric procedure, there has been a push to standardize practices and protocols to decrease opportunities for morbidity/mortality. Maternal obesity represents a potentially modifiable source of morbidity.