Presenting Author:
Jeffrey Bubley, B.A.
Principal Investigator:
Pedram Gerami, M.D.
Department:
Dermatology
Keywords:
Melanoma, Amelanotic Melanoma, Non-pigmented Lesions, Delayed Diagnosis, Superficial Spreading Melanoma, Nodular Melanoma
Location:
Ryan Family Atrium, Robert H. Lurie Medical Research Center
C8 - Clinical
Superficial Spreading and Nodular Amelanotic Melanoma, a Single-Institution Study
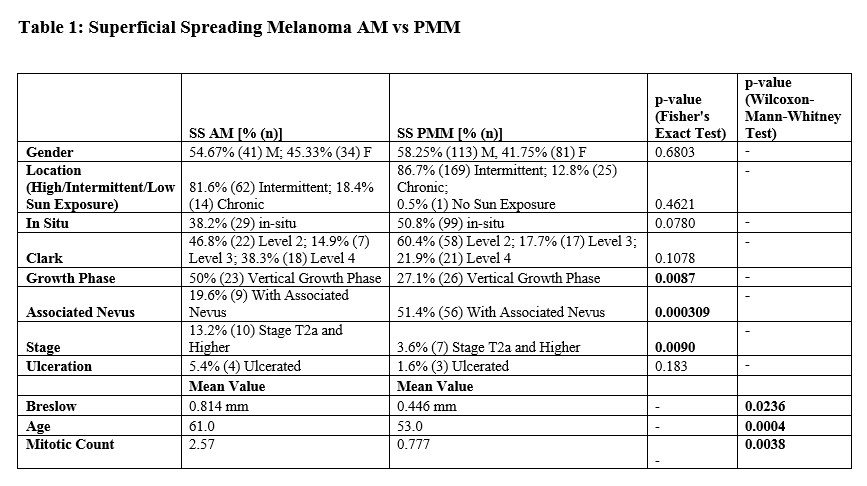
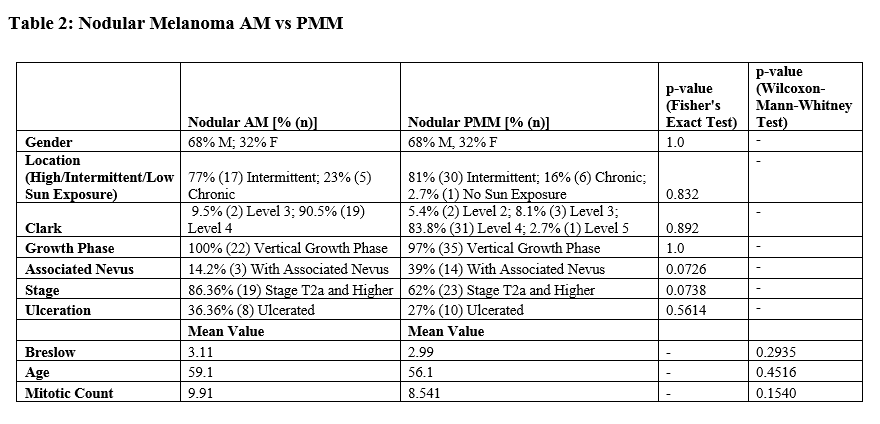
Background: Amelanotic melanomas (AM) lack typical dermatoscopic characteristics of pigmented melanoma and are typically diagnosed at a higher AJCC stage. Objective: To determine if superficial spreading amelanotic melanoma (SSAM) or nodular amelanotic melanoma (NAM) are mostly responsible for the advanced stage at the time of diagnosis. Methods: We identified 76 SSAM and 23 NAM cases. Control groups of superficial spreading pigmented melanomas (SSPM) (n=195) and nodular pigmented melanomas (NPM) (n=38) were used for comparison for multiple measures of tumor biology, as well as patient demographics. Results: SSAM presented with a greater mean Breslow depth (p=0.024) and stage (p=0.0090), were more likely to be in the vertical growth phase (p=0.0087), and in older patients (p=0.0004) than SSPM. There were no significant differences between the nodular cohorts. There was a higher proportion of nodular cases in the amelanotic versus the pigmented subgroups (p=9.0x10-6). Limitations: This is a single-institution study. Conclusion: More aggressive tumor biology and diagnostic delay likely both play a role in the adverse prognosis associated with AM. SSAM were more advanced at time of diagnosis compared to SSPM by all measured parameters. Improving our ability to recognize early SSAM represents a significant opportunity for intervention and improved outcomes in melanoma. Currently, the ABCDE criteria and other teachings on the identification of melanoma are most focused on the recognition of pigmented SSM. We encourage the need for better training in the identification of superficial spreading AM; likely dermoscopy will play a large role. Dermatologists should have a high index of suspicion for biopsying amelanotic lesions with any degree of atypia on clinical exam to avoid delays in diagnosis.