Presenting Author:
David Salzman, M.D.
Principal Investigator:
Diane Wayne, M.D.
Department:
Medical Education
Keywords:
simulation, mastery based learning, entrustable professional activities, capstone, medical students
Location:
Third Floor, Feinberg Pavilion, Northwestern Memorial Hospital
E10 - Education
EPA Simulation-Based Mastery Learning Capstone Course
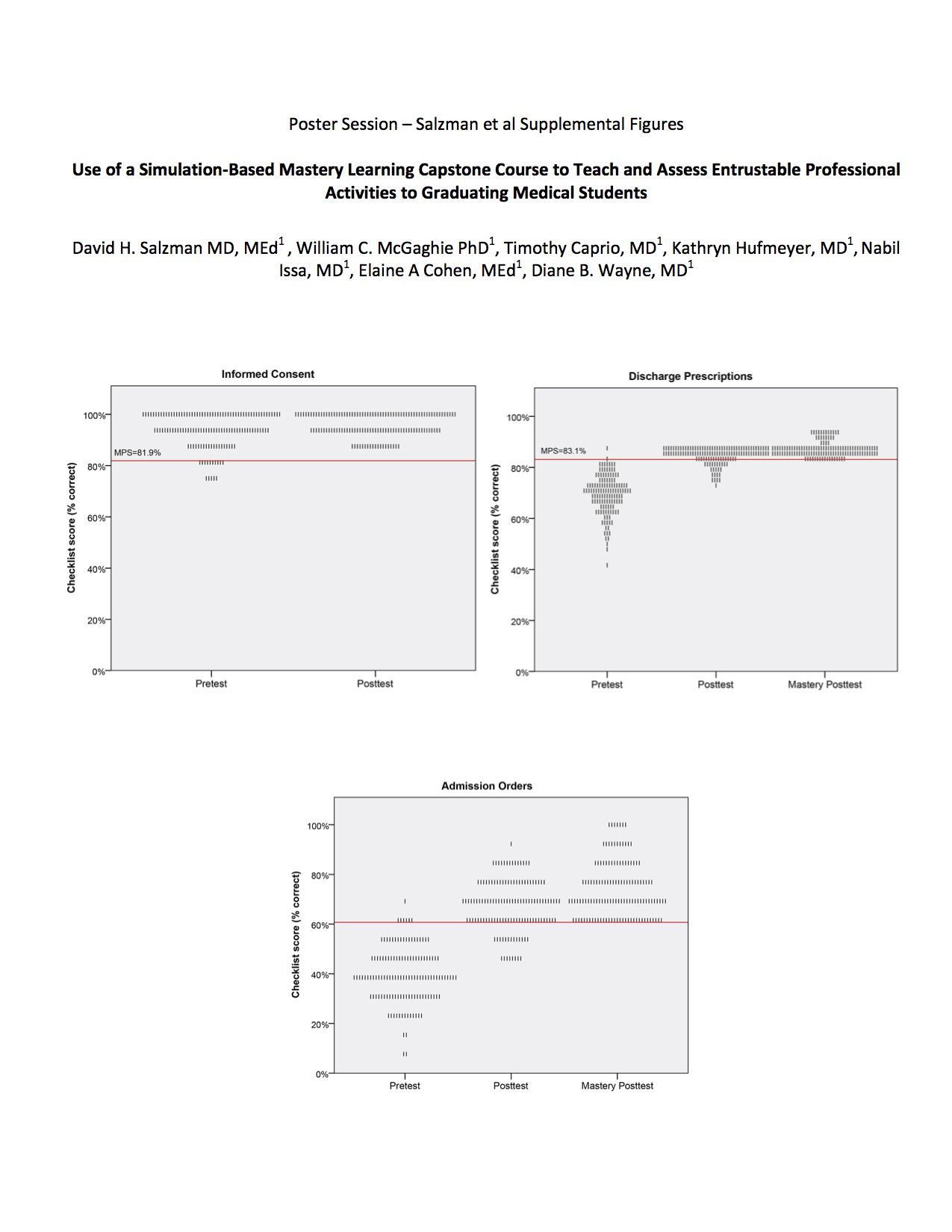
Ensuring that graduating students are prepared for the transition to residency, and can independently perform specific entrustable professional activities (EPA)s is critical(1-4). We developed and piloted a simulation-based, EPA focused, capstone course to assess graduating fourth year medical students’ readiness for residency(5). Given early success, we expanded the course to all graduating Northwestern medical students in the class of 2016. Students participated in a 6-station assessment of clinical skills examination (CSE) immediately prior to graduation. After pretesting, students received feedback about their performance and received 5 hours of scheduled time for deliberate practice of specific EPA skills. A minimum passing score (MPS) was established for 3 of the stations (informed consent, admission orders, and discharge prescriptions) prior to implementation of the course. Following practice, students completed a post-test assessment. Students that did not meet the MPS at the initial posttest returned to the simulation laboratory for additional deliberate practice and retesting until the MPS was met. A multidisciplinary panel of 12 clinical skills expert faculty reviewed prior performance of graduating medical students on the CSE and determined the MPS for each skill using the Angoff and Hofstee standard setting methods. The mean of the Angoff and Hofstee scores was used as the final MPS. The final MPS were set as informed consent - 81.9%, discharge prescriptions – 83.1%, and admission orders – 60.7%. 131/134 (98% of eligible) graduating students completed all protocol components and achieved mastery for the 3 stations. Three students did not complete the assessment due to scheduling difficulties. All students met or exceeded the MPS at final posttest. Those students who did not meet the MPS on initial post test required a maximum of one hour of additional practice per station prior to achieving the MPS on final posttest. This study shows that graduating medical students could not reliably perform clinical skills related to selected EPAs at baseline despite completing their standard undergraduate medical education curriculum. However, a focused simulation-based mastery learning experience improved performance and demonstrated competency as determined by a multi-specialty panel of expert faculty. References: 1. Core Entrustable Professional Activities for Entering Residency. http://members.aamc.org/eweb/upload/Core%20EPA%20Curriculum%20Dev%20Guide.pdf. Accessed February 10, 2016 2. Lypson ML, Frohna JG, Gruppen LD, Woolliscroft JO. Assessing residents’ competencies at baseline: identifying the gaps. Acad Med 2004;79(6):564-570. 3. Cohen ER, Barsuk JH, Moazed F, Caprio T, Didwania A, McGaghie WC, Wayne DB. Making July safer: simulation-based mastery learning during intern boot camp. Acad Med. 2013 Feb;88(2):233-9 4. Issa N, Fryer J, Swaroop M, McCarthy D, Wayne J, Meyerson S, DaRosa D. Surgery Boot Ca