Presenting Author:
Lindsay Thome, R.N.
Principal Investigator:
Jennifer Trainor, M.D.
Department:
Pediatrics
Keywords:
EPA, interprofessional communication, medical student, simulation
Location:
Third Floor, Feinberg Pavilion, Northwestern Memorial Hospital
E25 - Education
Assessing Performance of Medical Students in a Communication-Focused EPA
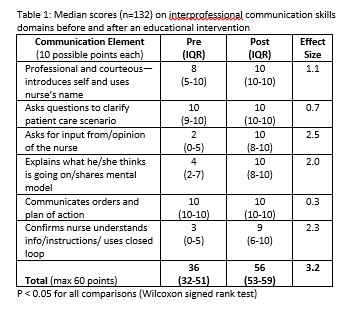
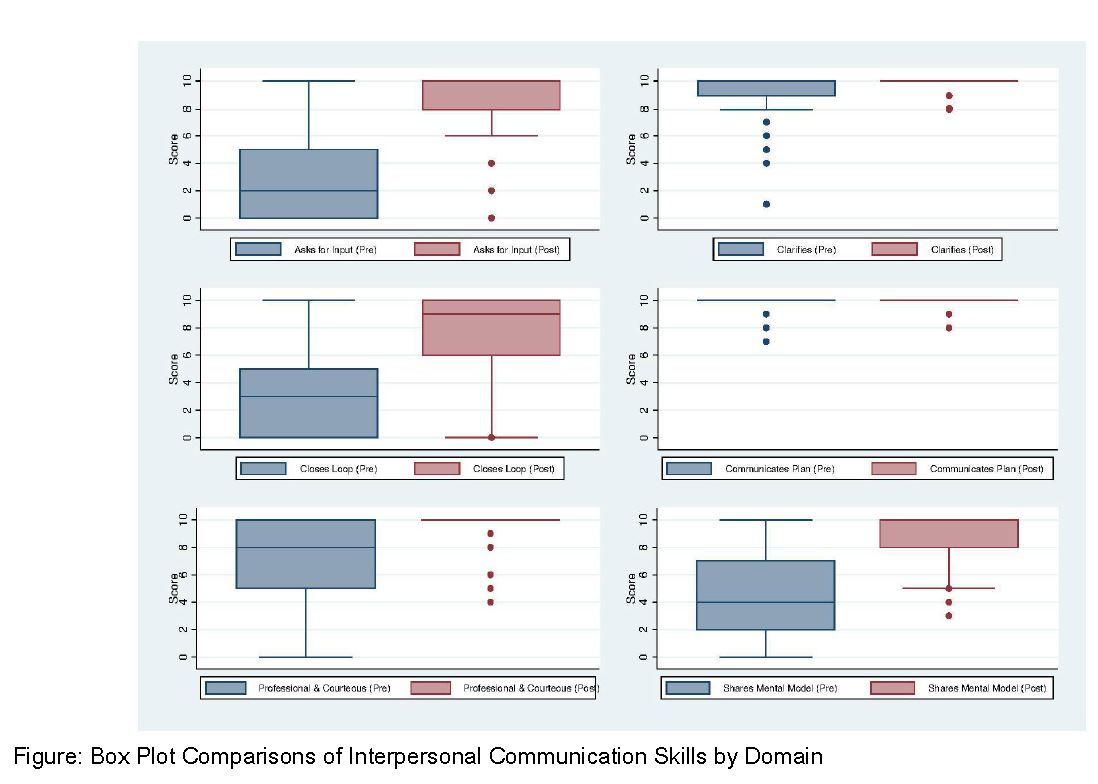
Background: Interprofessional communication is recognized as a key component of safe, effective team patient care. Little is known about medical student proficiency in answering nurse pages. Residents routinely answer pages unsupervised, however most have little prior experience and have received limited feedback on their skills. Objective: We sought to address this gap by 1) evaluating baseline interprofessional communication skills of graduating medical students responding to simulated nurse pages and 2) assessing the impact of an educational intervention on these skills. Design/Methods: As part of a capstone course, graduating students received verbal and written handoffs on mock patients during a clinical skills exam. Ten patient scenarios were developed as five pairs of pre and post cases, with similar medical content in each pair. Scenarios and checklists were piloted and revised iteratively. Six items were created to evaluate Entrustable Professional Activity (EPA) 9: collaborate as a member of an interprofessional team and scored as Done (2), Partially Done (1), or Not Done (0). Trained nurses provided scripted information at both pre and post-tests. After completing a pre-test, students attended a 1 hour interactive session on interprofessional communication and received individualized feedback on their skills. They then completed a skills post-test. Change in median scores and effect sizes were assessed using Wilcoxon Ranked Sign test and Cohen's d, respectively. Results: 132 students completed both pre and post-test assessments. Median scores were higher in all communication domains in the post-test as compared to the pre-test (Figure), with average effect size of 1.5 (Table 1). At baseline, students performed well in 3/6 domains: professionalism/courteousness, using clarifying questions, and communicating orders and a plan of action. However, students had lower scores for seeking input/opinion for the nurse, sharing their mental model, and employing closed loop communication. Conclusion(s): Despite completing all curricular requirements, graduating medical students did not reliably use communication best practices nor share their mental models in a way that would level the hierarchy across professions when answering pages. Following a focused communication intervention, students demonstrated meaningful improvement in these domains. Further study is needed on the best approach to fully prepare graduating medical students to participate in interprofessional teams.