Presenting Author:
Samantha Montag, M.S.
Principal Investigator:
Mercedes Carnethon, Ph.D.
Department:
Preventive Medicine
Keywords:
Objective Sleep, Sleep Duration, Sleep Maintenance, Incident Diabetes, Epidemiology
Location:
Third Floor, Feinberg Pavilion, Northwestern Memorial Hospital
PH40 - Public Health & Social Sciences
Association of sleep with incident diabetes: CARDIA Sleep Study
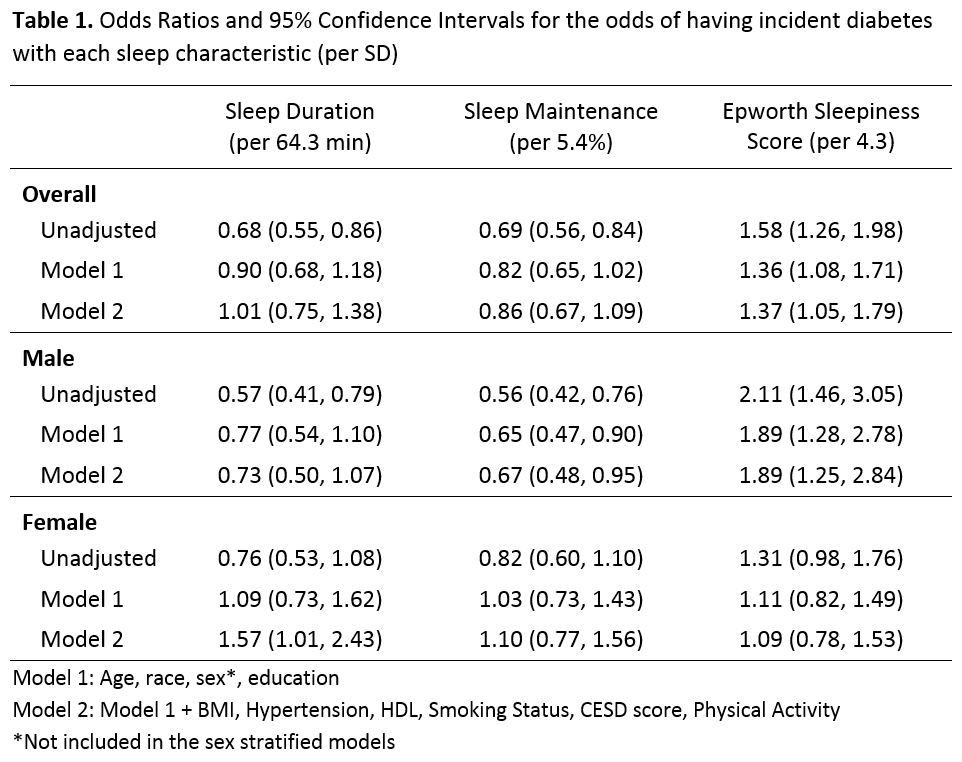
Background: Prior studies report a longitudinal association of short sleep and poor quality sleep with incident diabetes. However, most prior studies rely on self-reported sleep which is only moderately correlated with objective measures. It is not known whether these associations are present when objective measures are used. Objective: To examine the association of objectively-determined sleep duration and quality with the development of diabetes over 15 years in a population-based sample of black and white men and women. Methods: Coronary Artery Risk Development in Young Adults (CARDIA) Study participants at the Chicago, IL study center who wore wrist actigraphs (ActiwatchTM) twice (3 days each) between 2003-2005 and did not have diabetes at the 2000-2001 study visit were studied (n=594). Objectively measured sleep parameters (duration and maintenance) were averaged over 6 days. The Epworth Sleepiness Scale (ESS) is a self-reported measure used to assess daytime sleepiness. Diabetes was determined based on fasting glucose, oral glucose tolerance test, HbA1c, or diabetes medication use during follow-up examinations. Logistic regression analyses were used to calculate odds ratios and 95% confidence intervals per standard deviation of each sleep measure. Model 1 covariates included age, race, sex, and years of education. Model 2 additionally included BMI, hypertension, HDL, smoking status, CESD score, and total physical activity. We evaluated effect measure modification by race and by sex using multiplicative interaction terms. Results: Nearly half (N= 253, 42.6%) were male and 255 (42.9%) were black. At baseline (2000-2001), the average age was 40.1 (sd=3.6) years. On average, sleep duration was 6.1 hours (1.1) per day, and sleep maintenance, the percentage of the sleep period spent sleeping, was 88.9% (5.4). Participants reported an average ESS score of 7.5 (4.3). Over the 15 years, 78 (13.1%) participants developed incident diabetes, with rates higher among black participants (57, 22.4%) and women (46, 13.5%). In unadjusted pooled models, each sleep measure was associated with incident diabetes; however only the self-reported measure of daytime sleepiness was significant after adjustment for demographic and diabetes risk factors. Race did not modify the association of sleep with incident diabetes. However, sex did modify the associations between sleep and incident diabetes. Daytime sleepiness was associated with incident diabetes in males, but not females, while sleep duration was unexpectedly positively associated with diabetes risk among females but not males. Sleep maintenance was inversely associated with diabetes risk in males but not females. Conclusions: We observed very different associations of sleep characteristics with diabetes risk depending on whether sleep was assessed objectively or via self-report and the patterns were different in males and females. Future studies with larger samples are needed to confirm our findings.