Presenting Author:
Abigail Gilbert, M.D.
Principal Investigator:
Rowland Chang, M.D.
Department:
Physical Medicine and Rehabilitation
Keywords:
Knee osteoarthritis, rheumatoid arthritis, lifestyle physical activity, motivational interviewing, accelerometer, clinical trial
Location:
Ryan Family Atrium, Robert H. Lurie Medical Research Center
C101 - Clinical
The Improving Motivation for Physical Activity in Arthritis Clinical Trial
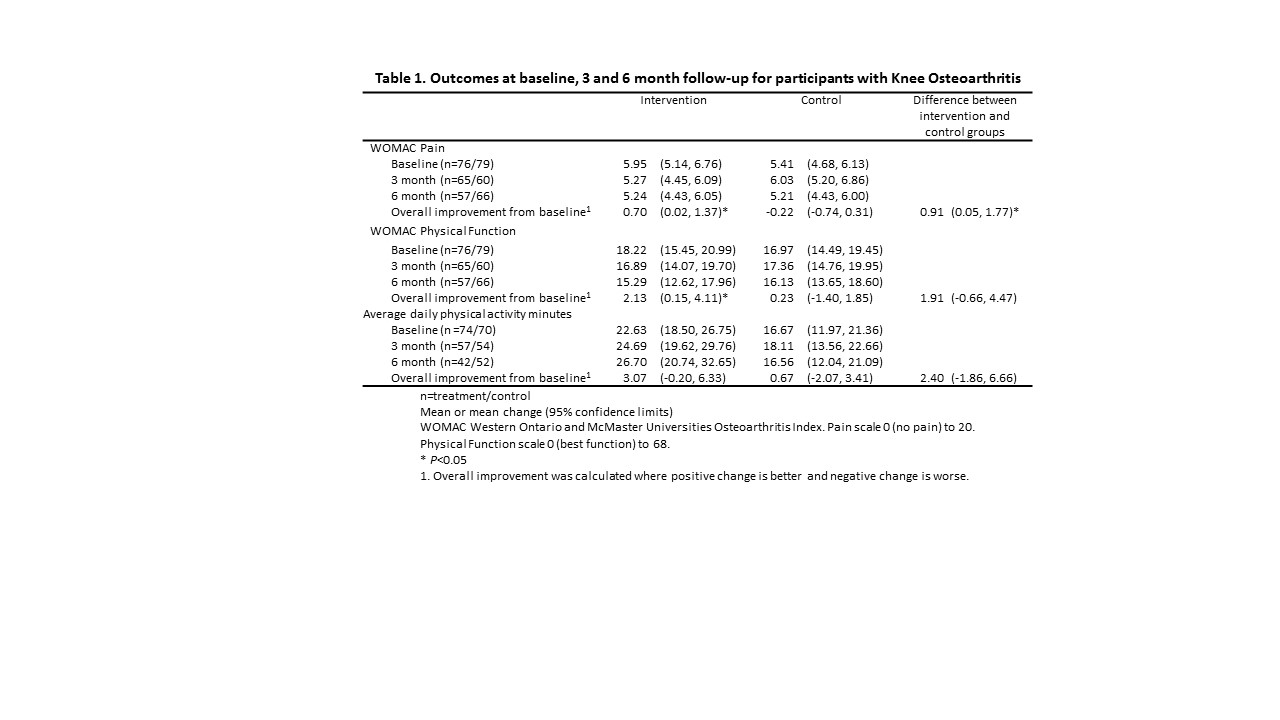
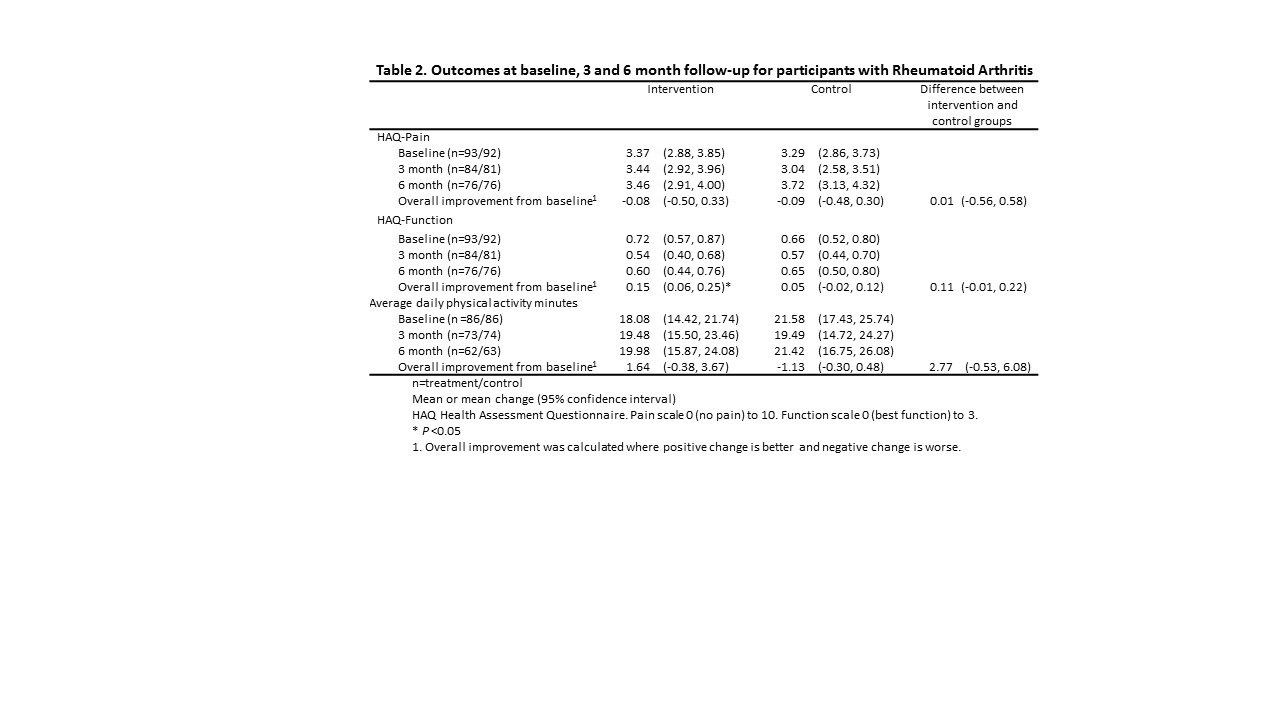
Background/Purpose: Insufficiently active adults experience reduced quality of life. Because half of adults with arthritis are physically inactive, we evaluated the additional effect of a motivational-interviewing based lifestyle physical activity intervention when added to physician-advice-only control group on pain and physical function in adults with knee osteoarthritis or rheumatoid arthritis (RA). Methods: Participants meeting American College of Rheumatology criteria for knee osteoarthritis or RA were randomized to physician-advise-only control or motivational-interviewing-based physical activity intervention group. For the motivational-interviewing intervention, participants met with a physical activity advocate who facilitated individualized physical activity goal setting and behavior change using motivational interviewing. Primary outcomes were pain and function evaluated by Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) for knee osteoarthritis and Health Assessment Questionnaire (HAQ) for RA at baseline, 3 months, and 6 months. Secondary outcome was accelerometer-measured moderate-to-vigorous physical activity (MVPA). Linear regression with generalized estimating equations (GEE) was used to evaluate the average intervention effect on changes in outcomes from baseline to 3 months and/or 6 months. Results: Participants included 155 adults with knee osteoarthritis (76 intervention, 79 control) and 185 adults with RA (93 intervention, 92 control). The knee osteoarthritis participants who received the motivational-interviewing physical activity intervention had WOMAC pain score improve by 0.91 points (95% CI 0.05, 1.77), WOMAC function improve by 1.91 points (95% CI -0.66, 4.47), and their average daily physical activity increased by 22.79 minutes/day (95% CI -18.45, 64.04) more than control. For the RA intervention group, HAQ function score improved by 0.11 (95% CI -0.01, 0.22) compared to controls. Conclusion: Motivational-interviewing-based physical activity intervention participants with knee osteoarthritis experienced significant improvement in pain compared to physician-advice-only controls. Both knee osteoarthritis and RA intervention participants demonstrated a trend towards improved physical function.