Presenting Author:
Principal Investigator:
Stephen Persell, M.D.
Department:
Medicine
Keywords:
Cardiovascular disease risk, care management, rheumatoid arthritis, risk factor assessment, statin
Location:
Third Floor, Feinberg Pavilion, Northwestern Memorial Hospital
PH25 - Public Health & Social Sciences
An Intervention to Improve Preventive Cardiology Practice in Rheumatoid Arthritis
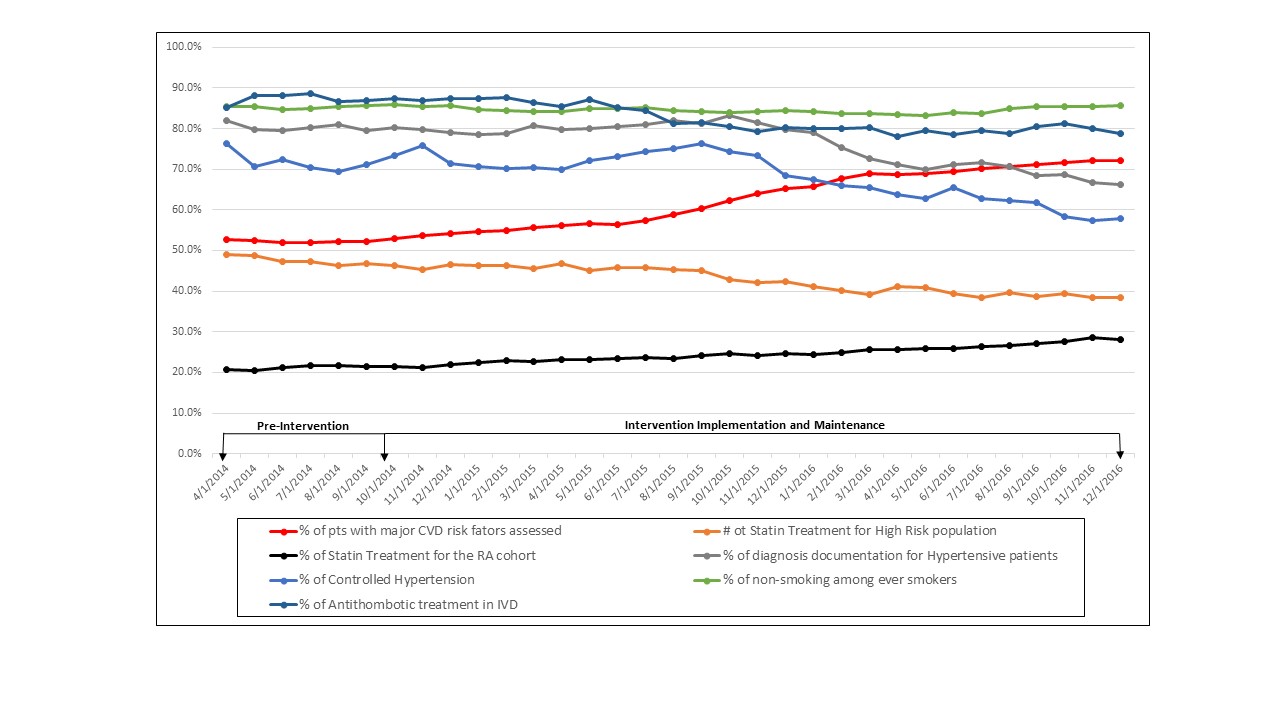
Background: Cardiovascular disease (CVD) is the leading cause of death in rheumatoid arthritis (RA). With RA, risk of CVD morbidity is increased 1.5-2.0 fold. Despite this burden, many RA patients do not have CVD risk factors assessed, and many opportunities exist to modify CVD risk. Methods: The study population, identified from EHR data included patients with a diagnosis of RA and at least 2 visits within 18 months. The intervention included: (1) clinician education, (2) point-of-care EHR clinical decision support, (3) provider feedback, and (4) care management. Rheumatologists approved outreach to patients with care gaps prior contact by a care manager. Eligible patients were mailed a letter that focused on applicable messages regarding their elevated CVD risk, missing lipid or glucose measurements, elevated blood pressure, or current smoking. Care managers then attempted to reach patients via telephone to follow-up. The assessed measures included the percentage of eligible patients who had: 1) assessment of all major CVD risk factors (blood pressure, cholesterol, diabetes screening, and a recorded smoking status, 2) moderate or high intensity statin among those with at least moderate CVD risk, 3) moderate or high intensity statin treatment among the overall population 40 to 75 years of age, 4) hypertension diagnosed among hypertensives, 5) controlled hypertension, 6) smoking status recorded as non-smoking among ever smokers, and 7) antithrombotic drug use in ischemic vascular disease. We used interrupted time series analysis to examine differences in the rates of change of these measures before and during the intervention. Results: At baseline, the study population (n=1267) was 57.1 years old (SD=14.3), 84% were female, and 54% were white. Rates of each measure before and after implementing the improvement activities are shown in the Figure. The percentage of patients with all major CVD risk factors assessed was 53.0% at the beginning of the implementation activities and rose to 72.2% by the end of the follow up period. The rate of increase for this measure was significantly greater during the intervention period compared to baseline, a difference of 0.74 percent increase per month (95% CI 0.28 to 1.19; P=0.0016). By the end of the study, more patients aged 40-75 years received a moderate or high intensity statin (21.6% to 28.2%) but the rate of change in the intervention period was not significantly different from baseline (P=0.13). No other measure increased during the intervention period. Conclusions: Implementing a multifaceted system-level intervention at one academic rheumatology clinic significantly improved CVD risk factor assessment but did not improve other preventive cardiology indicators. Future interventions are needed to identify the best ways to facilitate rheumatologist-to-primary care provider communication, harness clinician accountability, and improve awareness of RA’s increased CVD risk.