Presenting Author:
Taha Abdullah, M.S.
Principal Investigator:
Department:
Physiology
Keywords:
Placebo treatment, biomarkers, chronic pain, resting state functional connectivity (rsfMRI), periaqueductal grey (PAG), ... [Read full text]
Location:
Third Floor, Feinberg Pavilion, Northwestern Memorial Hospital
B160 - Basic Science
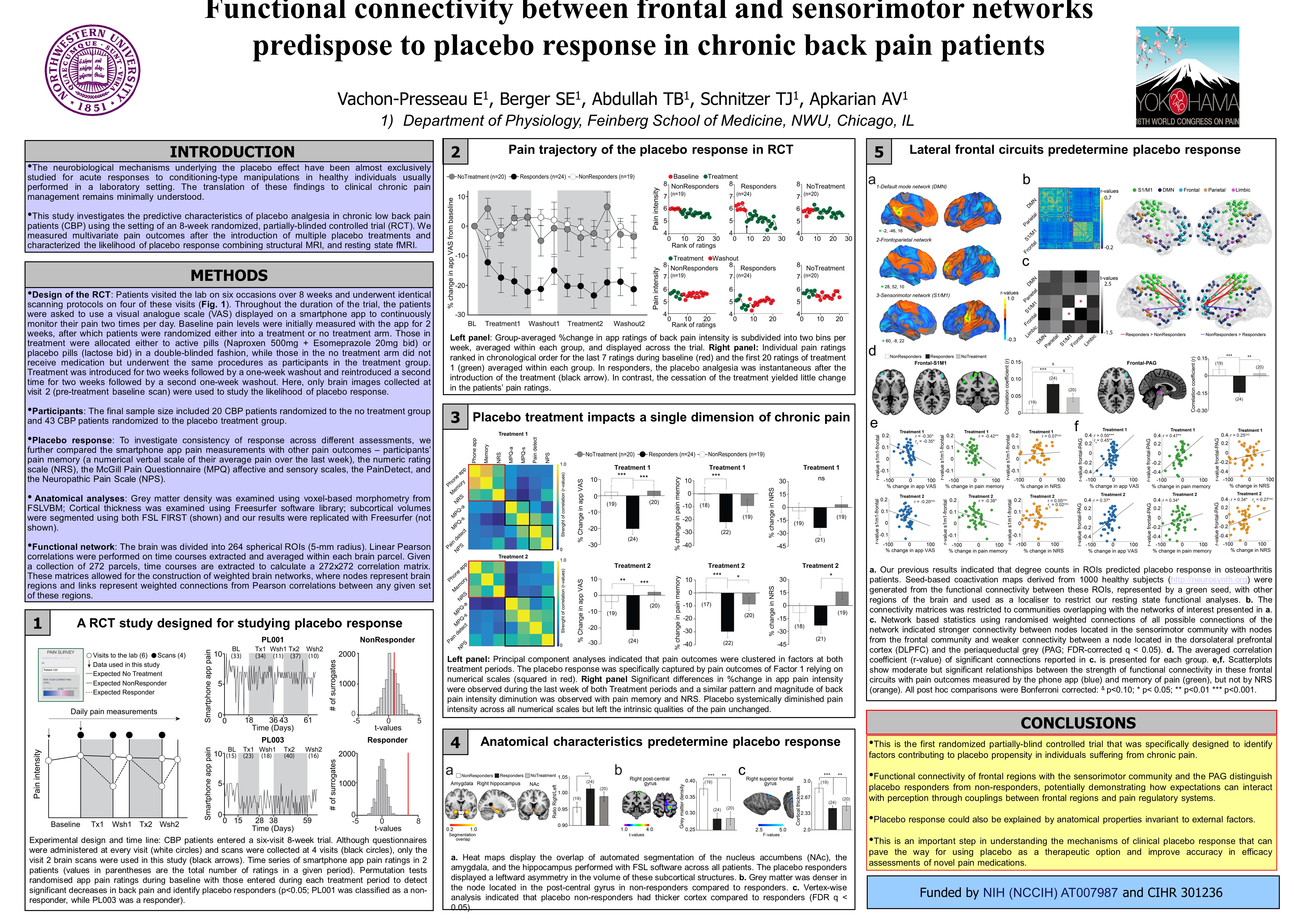
Functional connectivity between frontal-sensorimotor networks predispose placebo response in CBP.
Aim of Investigation: The placebo effect reflects an improvement in symptoms caused by receiving a sham treatment. Previous studies have demonstrated that the placebo response is associated with consistent brain activation. However, the neural mechanisms underlying placebo’s therapeutic benefit in clinical populations remain to be determined. Here, we studied functional and anatomical brain properties predisposing chronic back pain patients (CBP) to long-lasting placebo response in a randomized double-blinded clinical trial. Methods: We enrolled 69 CBP patients and randomized them to one of 3 arms: placebo (n=45), no treatment (n=20), and positive control (n=4). After a two-week baseline period, participants were treated for a two-week period, followed by a one-week washout, and this regimen was then repeated once more. Participants underwent functional and anatomical brain scans at the beginning and the end of each treatment period. Additionally, participants were asked to continuously monitor their pain and mood twice a day using a smartphone application. Here, we only present the data before any treatment was administered. Participants were classified as a responder based on a permutation (10,000 sampling permutations) test between the pain ratings during baseline and the ones during each treatment period. Resting state functional connectivity (FC) was used to identify propensity to placebo response. Brain networks were constructed from Pearson correlations of resting state bold signals between 264 nodes. A modularity analysis was performed to segregate strongly connected nodes into communities. We restricted our analyses to three networks of interest: the default mode network (DMN); the frontal network, and the sensorimotor network (S1/M1). The FC quantified as Pearson correlations r-values within and between networks was compared between responders and non-responders. Results: The permutation test revealed that 16 CBP patients responded during the first treatment period and an additional 8 responded during the second treatment period (responders: 24). The average FC (r-values) between nodes of the frontal network with nodes of the sensorimotor network were significantly stronger in placebo responders compared to nonresponders (t(1,43) = 2.56; p =0.014). Network-based statistics using permutation tests on FC (r-values) confirmed stronger connections between nodes located in the sensorimotor network with nodes from the frontal network (FDR-corrected; p<0.00001). Conclusions: We demonstrate that placebo response in clinical trials may over time. We further demonstrate that CBP patients showing a propensity to respond to either treatment periods have stronger FC between frontal and sensorimotor networks at baseline. This confirms our previous results demonstrating the importance of the frontal network, involved in expectation and top-down modulation, and its specific communication with sensorimotor network as a mechanism of placebo response