Presenting Author:
Rafael Confino, B.S.
Principal Investigator:
Mary Ellen Pavone, M.D.
Department:
Obstetrics and Gynecology
Keywords:
cancer outcomes, fertility preservation, oncofertility
Location:
Ryan Family Atrium, Robert H. Lurie Medical Research Center
C67 - Clinical Women's Health Research
Long term outcomes in cancer patients who pursued fertility preservation
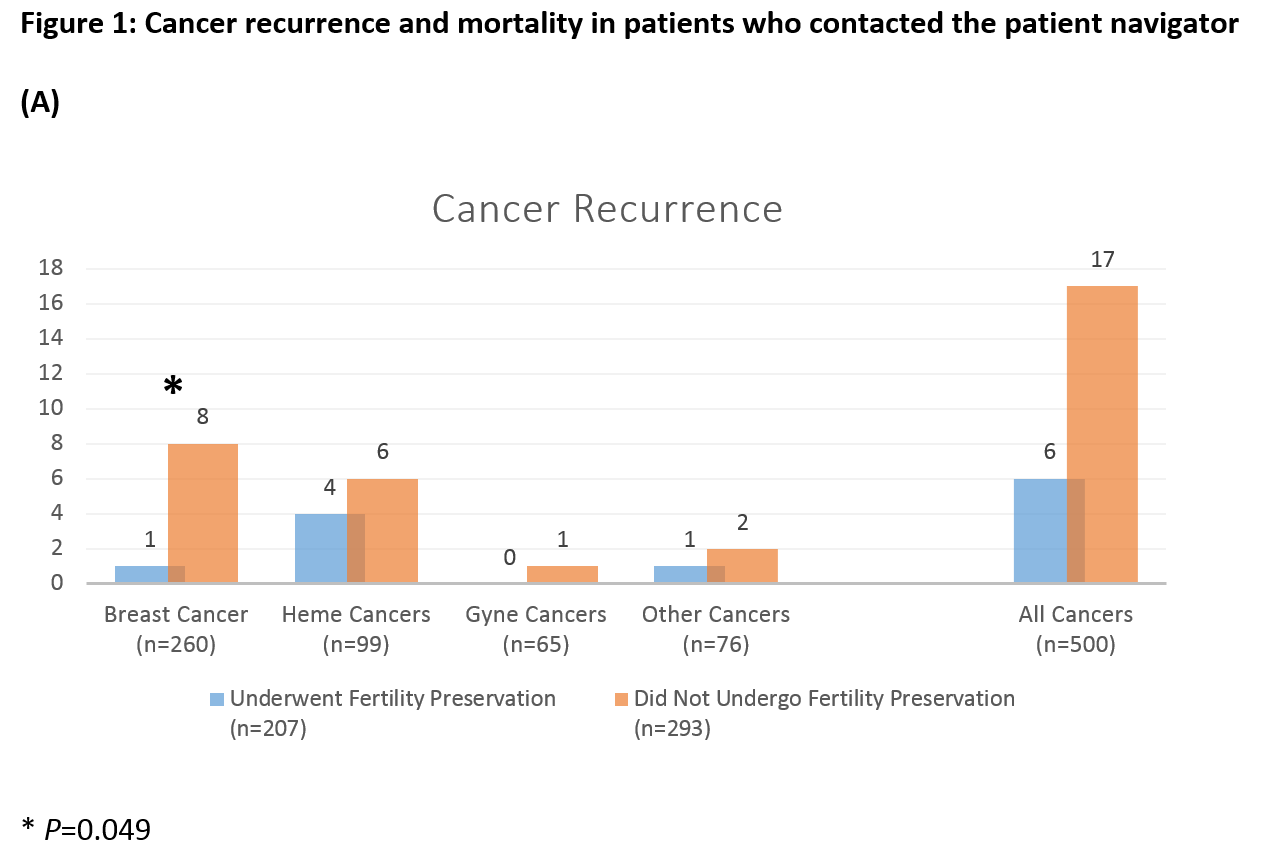
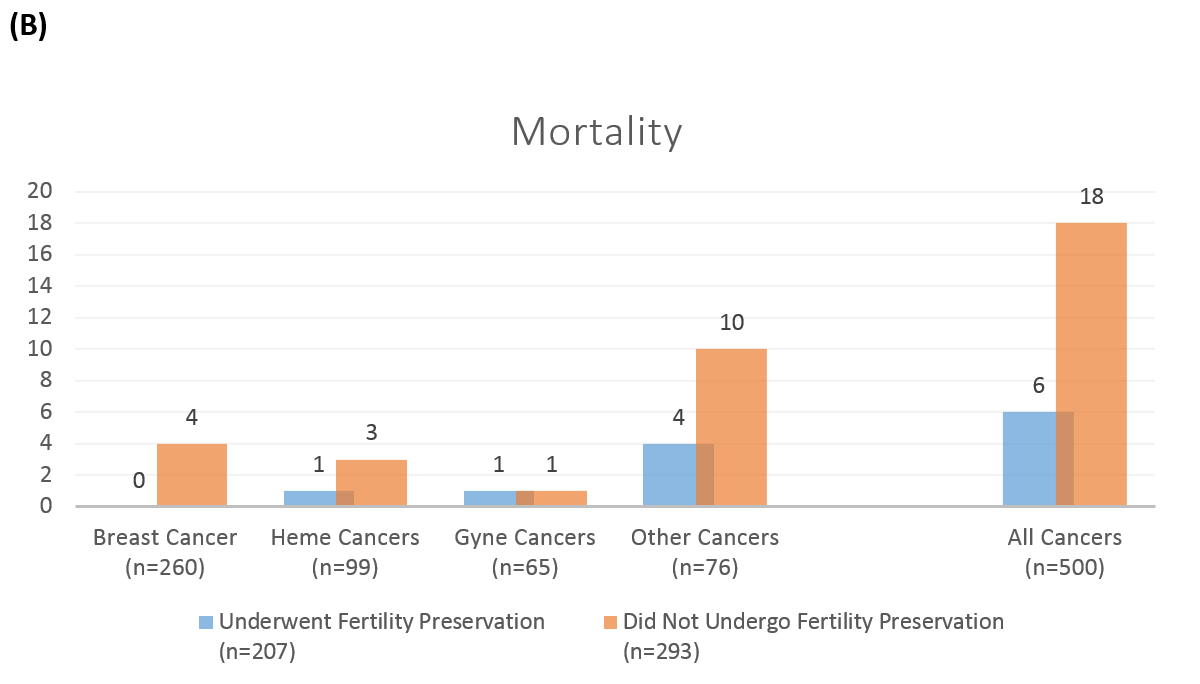
Background: Although fertility preservation counseling prior to cancer treatment has been mandated by several national societies, referral rates are low. This may be partly because of concerns that fertility preservation may delay treatments and worsen cancer outcomes. Objectives: We quantified time to cancer treatment and outcomes in patients who did and did not pursue fertility preservation. We also compared cycle-specific and random-start stimulation protocols, and described reproductive outcomes following cancer treatment. Study Design: Retrospective cohort of patients who contacted the fertility preservation patient navigator at a single urban academic institution. Data was analyzed by chi-square test and linear or logistic regression. Results: 500 patients met inclusion criteria, of which 41.4% elected fertility preservation. The median number of days to cancer treatment after initial consultation was 33d in the fertility preservation group and 19d in the group that declined (P = 0.000). There was no difference in cancer recurrence or mortality between groups. A cycle specific protocol was used in 175 fertility preservation patients while 23 had random-start. There were no differences in stimulation parameters, outcomes or days to next cancer treatment. 19 patients returned to use cryopreserved gametes, of which 8 used a gestational carrier, resulting in 11 live births. 16 patients in each group experienced a spontaneous pregnancy. Conclusions: Fertility preservation is both safe and efficacious for eligible cancer patients. Only 10% of patients returned to use cryopreserved specimens, and almost half used a gestational carrier, suggesting the need for further research into reproductive decision-making in cancer survivors. Comment: This is the first study to demonstrate that, compared to patients that did not elect fertility preservation, cancer patients who had ovarian stimulation for fertility preservation had only minimal delays to initiation of cancer treatment, which is unlikely to be clinically significant. Other papers that examined this topic either only included patients with breast cancer or did not have a comparison group. Importantly, we found that there was no increase in cancer recurrence or mortality rates in patients who elected fertility preservation. Additionally, for patients who pursued fertility preservation, there were similar IVF cycle outcomes between cycle-specific and random-start protocols, and the random-start protocol did not significantly shorten time to next cancer treatment. Finally, the small number of patients that did return to use cryopreserved embryos had satisfactory live birth rates.