Presenting Author:
Erik Ladomersky, Ph.D.
Principal Investigator:
Department:
Neurological Surgery
Keywords:
Glioblastoma, Immunosuppression, Immunotherapy, IDO1, Treg, Tryptophan
Location:
Third Floor, Feinberg Pavilion, Northwestern Memorial Hospital
B99 - Basic Science
Combination therapy with IDO1 inhibitor for enhancing glioblastoma treatment efficacy
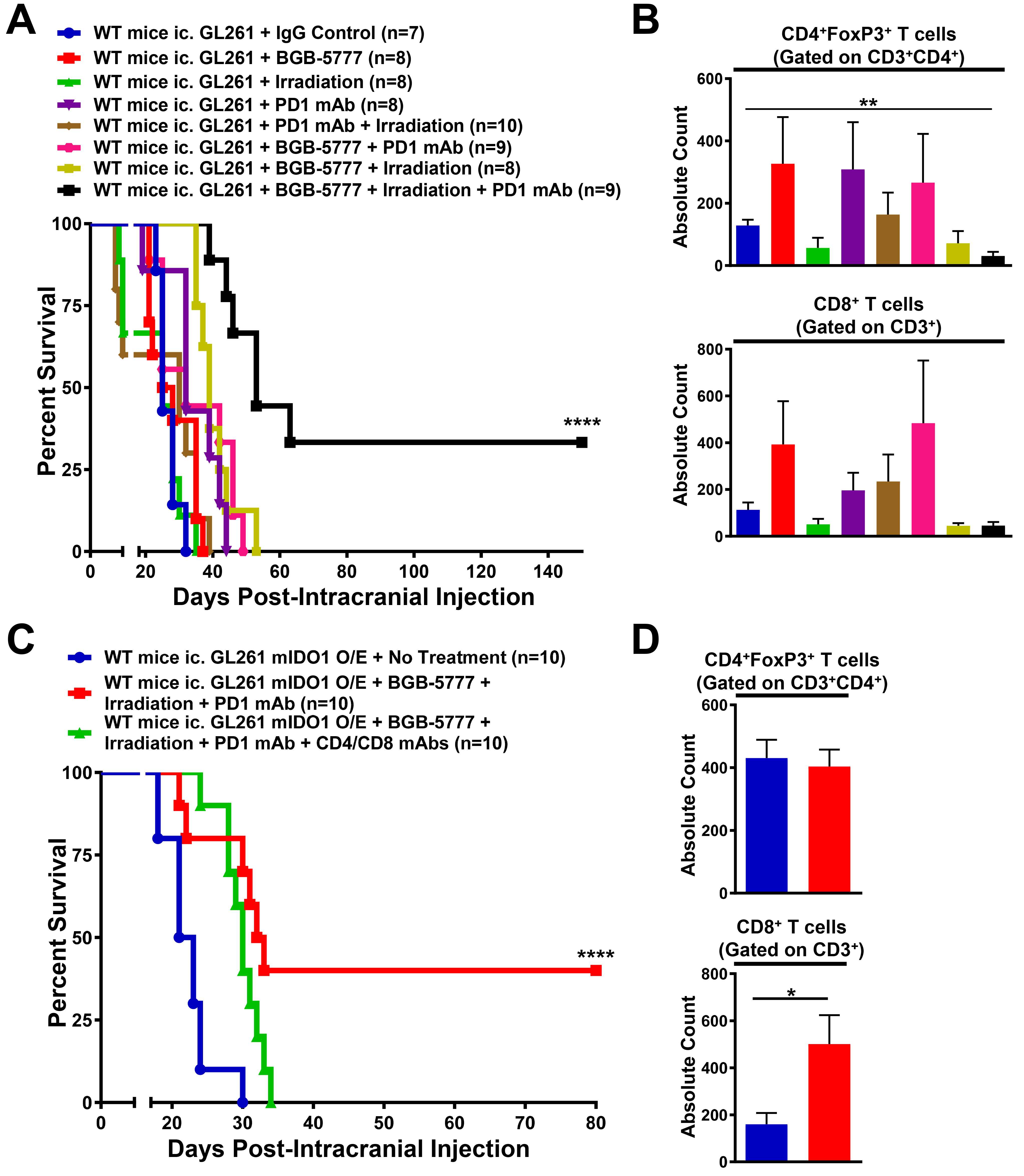
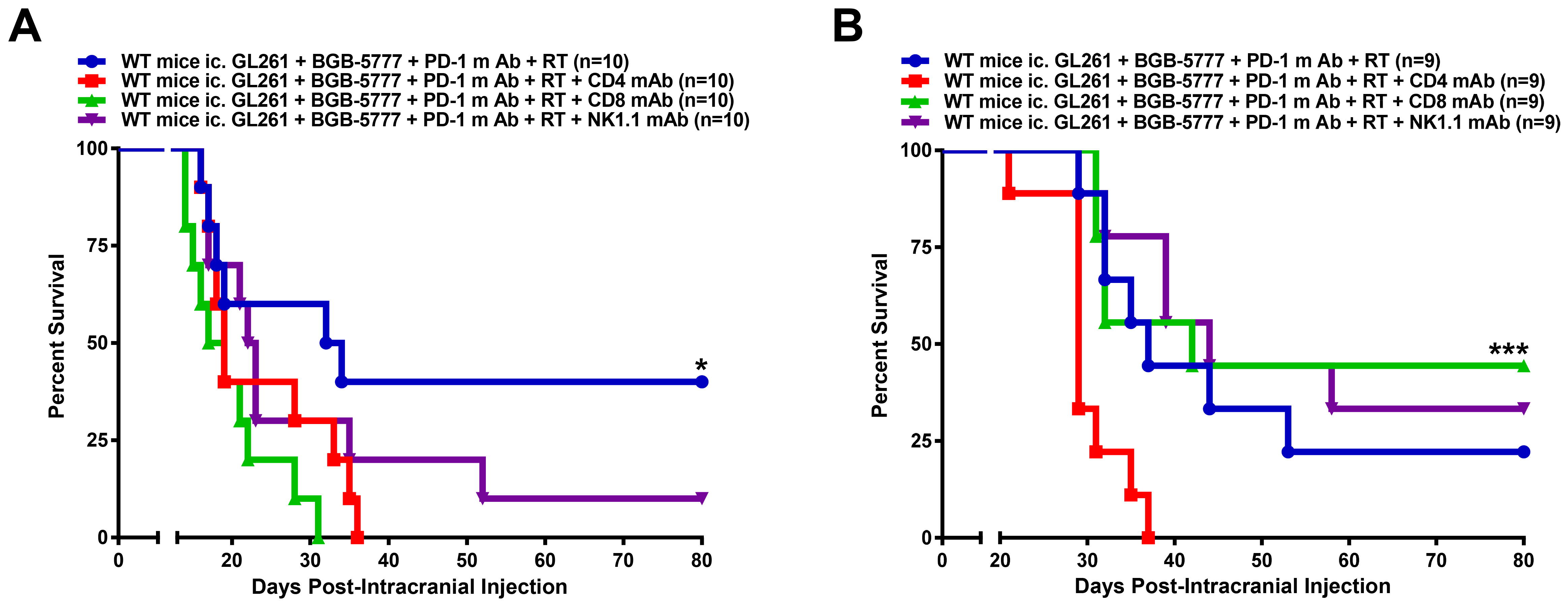
Glioblastoma (GBM) is a fatal primary brain tumor that, even after maximum surgical resection, radiotherapy (RT) and chemotherapy, is associated with a median overall survival (OS) of 14.6 months. Combinatorial treatment approaches that simultaneously address tumor growth, as well as the immunosuppressive microenvironment, may prove to be more effective than current clinical strategies. This work aims to determine the therapeutic efficacy of combining the novel, pharmaceutical-grade IDO1 enzyme inhibitor, BGB-5777, with PD-1 blockade and/or whole brain radiation, in a syngeneic, immunocompetent mouse glioblastoma model. Mice were intracranially-engrafted 2×105 GL261 cells to recapitulate brain tumors. At 14 days post-intracranial injection (post-ic.), mice with well-established GBM were treated with 2Gy whole brain radiotherapy (RT) for 5 days (n=8), 4 doses of PD-1 mAb (J43) given every 3 days (n=8) or 100mg/kg BGB-5777, BID, for 4 weeks (n=10), with a median OS of 25, 32, and 26.5 days, respectively. Mice treated with dual therapy including RT and PD-1 mAb (n=10), RT and BGB-5777 (n=8), or PD-1 mAb and BGB-5777 (n=9), had a median OS of 30, 39, and 32 days, respectively. All mice treated with mono- or dual-therapy succumbed to tumor burden. In contrast, mice treated with concurrent RT, PD-1 mAb and BGB-5777 (n=9) showed a significant increase in median OS to 53 days (P<0.0001), with 33% of mice demonstrating a durable survival benefit (>150 days). A day 21 post-ic. T cell analysis showed a significant decrease in GBM-infiltrating Treg levels in mice treated with triple therapy vs. control mice (P<0.01). Unexpectedly, mice with GBM engineered to overexpress mouse IDO1 and treated with triple therapy showed a proportion of durable survivors (40%) vs mice with unmodified GBM and treated similarly (P<0.0001). Interestingly, the survival effects were independent of immunosuppressive Treg levels, but associated with increased cytolytic T cell levels. Importantly, mice treated with the triple therapy and co-administered CD4 (n=9) or CD8 (n=9) T cell-depleting mAb at 5 days post-ic., both showed a decrease in OS (18 days and 19 days, respectively, P=0.02), while mice treated with CD4 or CD8 depleting mAb, beginning at 14 days post-ic., showed decreased OS in CD4 T cell (29 days, P<0.001)-, but not CD8 T cell-depleted mice, when compared to non-depleted mice treated with the triple therapy, alone. These data suggest that, early GBM infiltration by CD8+ T cells and constant recruitment of CD4+ T cells, is required for immunotherapeutic efficacy. For the first time, our data indicate that combining RT, with PD-1 and IDO1 blockade, synergistically increases OS against well-established mouse GBM. These data suggest that, utilizing radiation to induce immunogenicity and/or inflammation in GBM, while co-inhibiting tumor-induced immunosuppression, is a rational and potentially clinically-beneficial pursuit.