Presenting Author:
Elaine Cohen, MEd
Principal Investigator:
Jeffrey Barsuk, M.D.
Department:
Medical Education
Keywords:
competency, central venous catheter, mastery learning, simulation, qualitative research
Location:
Third Floor, Feinberg Pavilion, Northwestern Memorial Hospital
E7 - Education
Healthcare Providers’ Understanding of Competency Requirements in Central Line Insertion
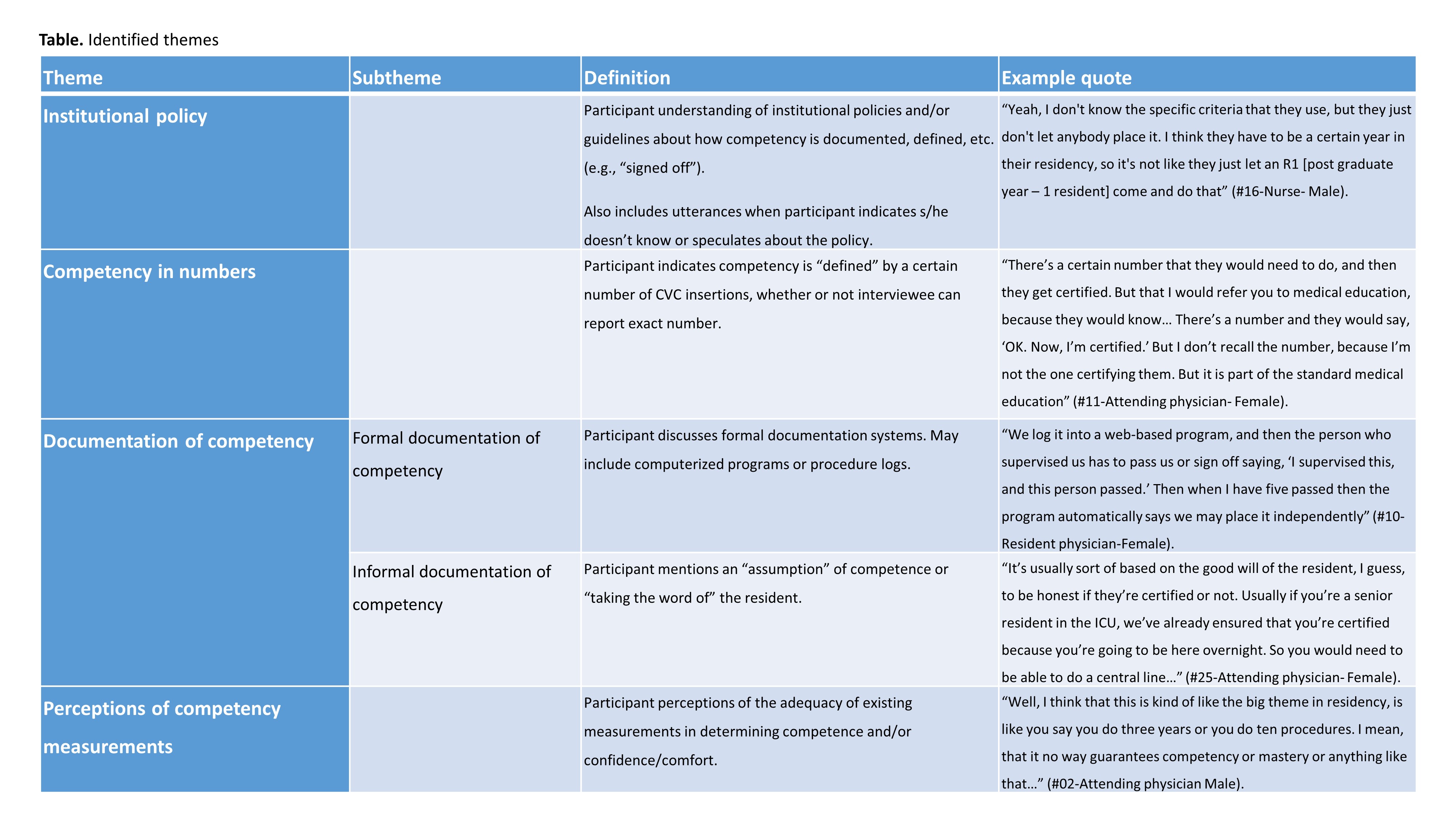
Purpose Studies show that trainees do not feel comfortable and lack the skills and confidence to perform common bedside procedures. Regulatory bodies often require a set number of procedures to determine competence, yet medical providers’ awareness of competency guidelines are less well known. This studied aimed to identify practices regarding documentation of competency in central venous catheter (CVC) insertion and explore healthcare providers’ awareness and understanding of those practices at their institutions. Method The authors performed a qualitative study at Veterans Affairs Medical Centers (VAMCs) from February to December 2014 as part of a larger project related to the dissemination of a simulation-based CVC insertion course. Two authors performed interviews with hospital staff (including attending physicians, nurses, and residents) at selected VAMCs. Recordings of interviews were transcribed, coded, and analyzed by using constant comparative techniques. Results Twenty-six participants (14 attending physicians, 2 resident physicians and 10 nurses) were interviewed at six VAMCs. When asked how someone might know if a physician is competent or “signed off” in CVC insertion, several themes emerged from all types of participants regarding their institutions’ existing practices (Table). The majority of participants knew of a “count-based” system, yet gave inconsistent responses regarding the required number of procedures to demonstrate competence. Most participants were aware of a formal system used at their institution to document competency, yet many relied on informal means of verifying competence. Participants reported concern about the reliability of these policies and measures of competence. Conclusion This study demonstrates that healthcare providers’ knowledge and perceptions about institutional requirements for procedural competency varied widely. Further study is needed to develop reliable assessments that yield valid decisions about procedural competence, consistent across institutions.