Presenting Author:
Kristin Kan, M.D. M.S.c
Principal Investigator:
Kristin Kan, M.D.
Department:
Pediatrics
Keywords:
child health, children with special health care needs, adverse childhood experiences
Location:
Third Floor, Feinberg Pavilion, Northwestern Memorial Hospital
PH32 - Public Health & Social Sciences
Adverse Experiences among Children with Special Health Care Needs
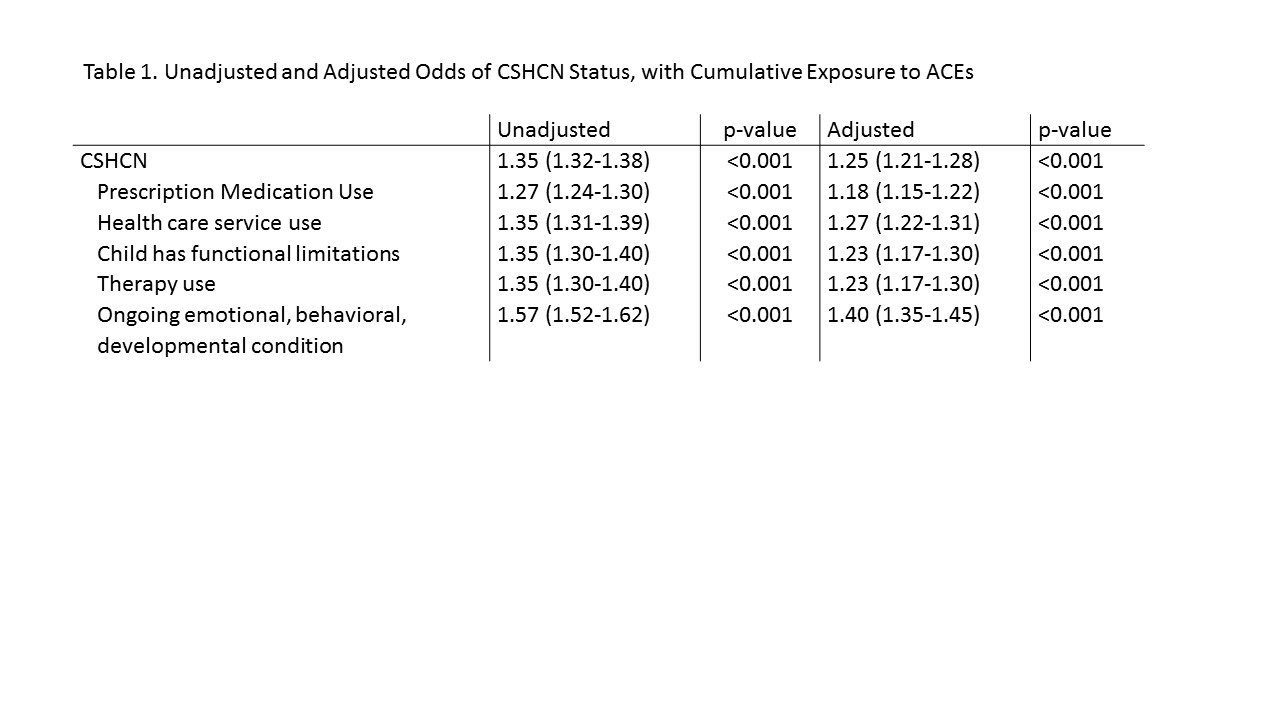
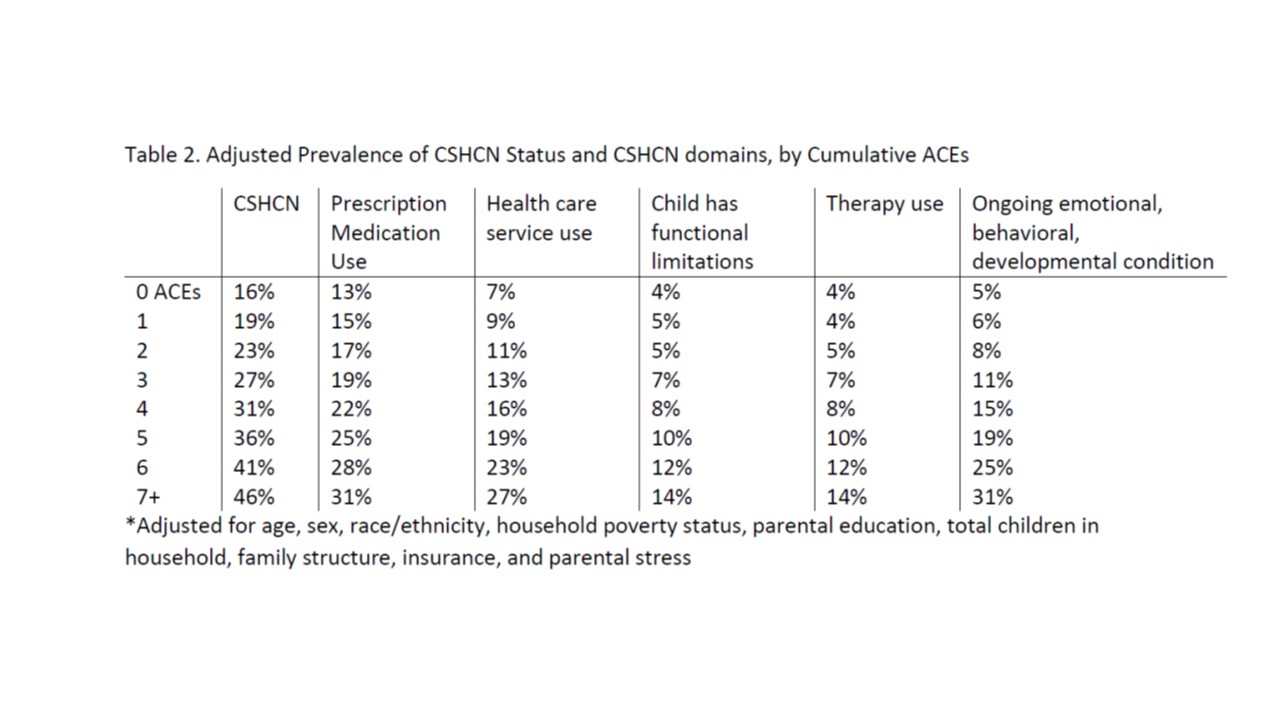
Background: Experiences in childhood shape health and well-being throughout the life course. Understanding linkages between adverse childhood experiences (ACEs; e.g., experiences of abuse, neglect, and family dysfunction) and the development of chronic conditions (e.g., asthma and obesity) in children is an emerging area of study. Children with special health care needs (CSHCN) are a particularly vulnerable group of children with a chronic condition and disproportionately high health service use. We examined the association between adversity and development of disease among CSHCN, and possible mitigating effects of coping. Objective: Evaluate whether a dose-response relationship exists between ACEs and being a CSHCN and whether emotional regulation (i.e., coping effort) mediates the relationship between ACEs and CSHCN status. Methods: A cross-sectional analysis of a sample of 91,129 children, 0-17 years old, in the 2011 National Survey of Children’s Health, a nationally representative survey of U.S. households with children. We compared the odds of being a CSHCN based on cumulative ACE exposure (among 9 possible ACEs). Multivariable logistic regression models were constructed for being CSHCN (main outcome) and 5 aspects of CSHCN (secondary outcomes)—prescription medication dependence, increased health care use, having functional limitations, dependence on specialized therapies, and having an ongoing emotional, behavioral, or developmental disorder. A mediation analysis was also used to assess the hypothesis that differences in the odds of being a CSHCN is partially explained by the lack of emotional regulation when exposed to ACEs. Results: Children with 4 or more ACEs were more likely to have an income below 133% FPL, be in a single mother household, have public insurance, live in a family with greater levels of parental stress, and be older, than children with 3 or fewer ACEs (all p<0.001). The odds of being a CSHCN increased with each accumulated ACE (adjusted odds ratio: 1.25, 95% confidence interval: 1.21-1.28). The adjusted prevalence of being a CSHCN with no ACEs was 16%, compared with 46% among children with exposure to 7 or more ACEs. Among children with 7 or more ACEs, the adjusted prevalence of prescription medication dependence or having an ongoing emotional, behavioral, or developmental condition was 31%. The lack of emotional regulation mediated the association between ACEs and CSHCN status. Conclusion: A dose-response relationship exists between ACE exposure and being a CSHCN, mediated by the lack of emotional regulation in a child. This study provides an initial exploration into how emotional regulation might mitigate the development of special care needs for children exposed to ACEs.