Presenting Author:
Claire Gerber, Ph.D.
Principal Investigator:
Tamara Isakova, M.D.
Department:
Medicine
Keywords:
racial disparities, kidney disease, CKD, ESRD
Location:
Third Floor, Feinberg Pavilion, Northwestern Memorial Hospital
PH29 - Public Health & Social Sciences
Association of Race with Development of CKD in ACCORD
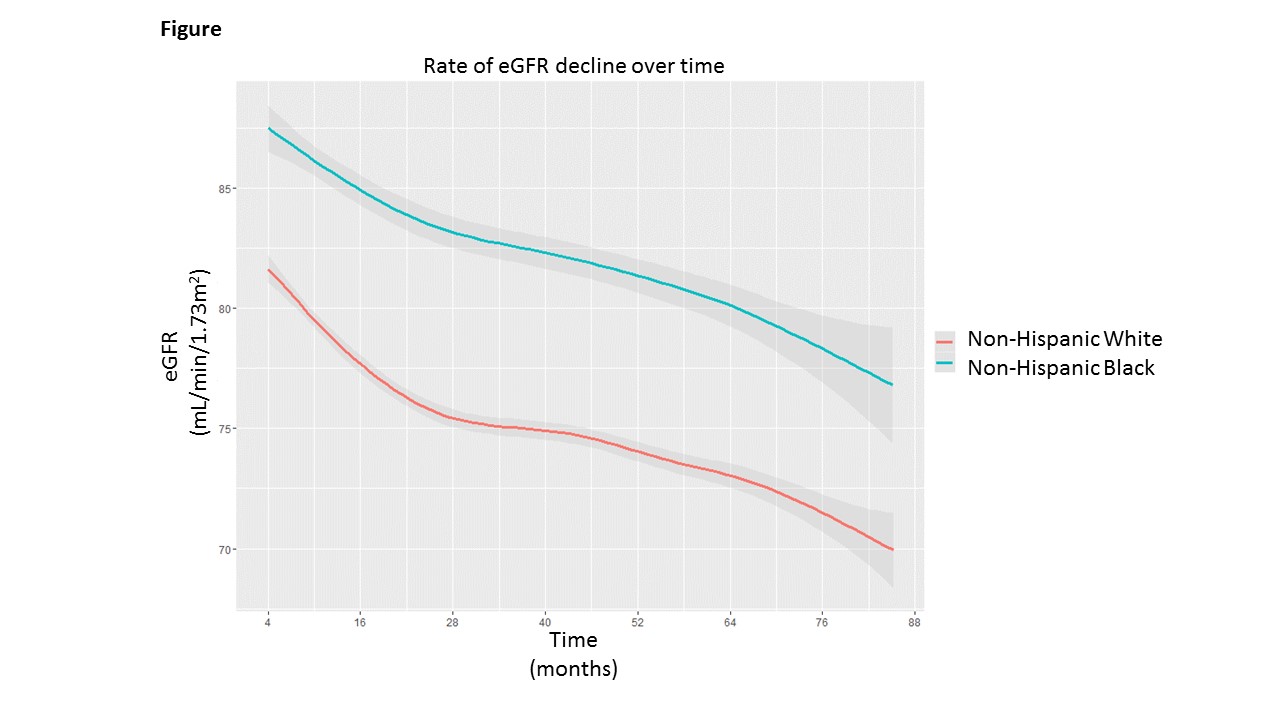
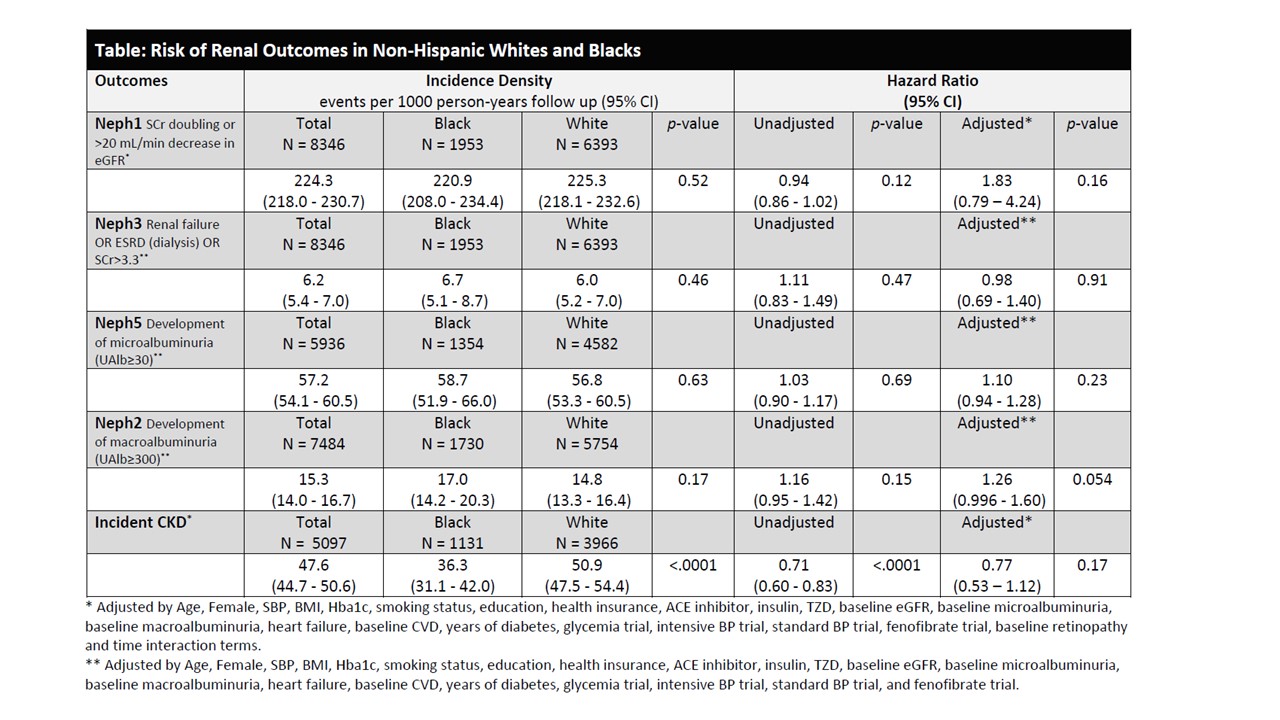
Background: Type 2 diabetes and its complications, including CKD, disproportionately affect blacks. Compared to whites, diabetic blacks are more likely to have macroalbuminuria and are at 50% higher risk of progression to ESRD. Differential access to care is a likely contributor to racial disparities in development and progression of CKD in diabetes. Studies of patients with long-standing diabetes and CKD revealed that racial differences in risk of CKD progression persist even with comparable delivery of care. It remains uncertain if delivery of equitable health care prior to onset of CKD will reduce disparities in development and progression of CKD in the diabetic population. Methods: ACCORD, an RCT, evaluated the effects of glycemic, lipid and blood pressure control on major cardiovascular disease events in 10,251 patients with type 2 diabetes and low prevalence of CKD at baseline. The trial was stopped early due to higher mortality in the intensive glycemic therapy group. To determine whether, within the context of an RCT and standardized medical care, racial differences in development and progression of CKD persist in patients with diabetes and low prevalence of CKD, we performed post-hoc analyses (n=8346) that examined associations of black race with longitudinal change in eGFR from month-4 study visit, incident CKD (new onset of eGFR<60 ml/min/1.73m2 that represented a ≥25% decrease from baseline in an individual with eGFR≥60 ml/min/1.73m2 and no microalbuminuria at baseline) and trial-specified nephropathy outcomes (serum creatinine doubling or >20 mL/min/1.73m2 decrease in eGFR, renal failure or ESRD, development of microalbuminuria or macroalbuminura). Race was self-reported. Results: We studied 1953 non-Hispanic blacks and 6393 non-Hispanic whites. Blacks had significantly longer duration of diabetes in comparison to whites (11.3±7.9 vs 10.6±7.5 years, p-value=0.001). Baseline eGFR was significantly higher in blacks (94.6±22.9 mL/min/1.73m2) in comparison to whites (88.2±21.8 mL/min/1.73m2, p-value<0.0001). During a mean follow-up of 4.6 years with comparable access to care, adjusted rate of eGFR decline over time was not different in black and white participants (Figure, p-value=0.16). Unadjusted rate of incident CKD was significantly higher in whites compared to blacks, but the unadjusted rates for nephropathy outcomes were not significantly different between races (Table). Multivariable-adjusted Cox models showed no differences in risks of development of incident CKD or nephropathy outcomes (Table). Conclusions: Race was not associated with accelerated development and progression of CKD in ACCORD participants who received standardized medical care. Although our findings are limited by short duration of follow-up, the results suggest that equitable health care delivery for patients with diabetes may reduce racial disparities in diabetes-associated CKD.