Presenting Author:
Reiping Huang, Ph.D.
Principal Investigator:
Jonah Stulberg, M.D.
Department:
Surgery
Keywords:
Age effect, surgical outcomes, surgical complexity
Location:
Third Floor, Feinberg Pavilion, Northwestern Memorial Hospital
PH60 - Public Health & Social Sciences
Patient Age, Surgical Complexity, and Postoperative Outcomes following Elective Surgery
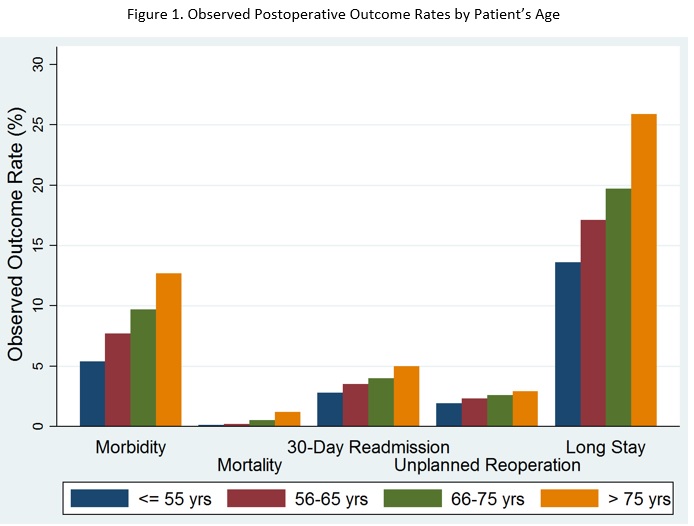
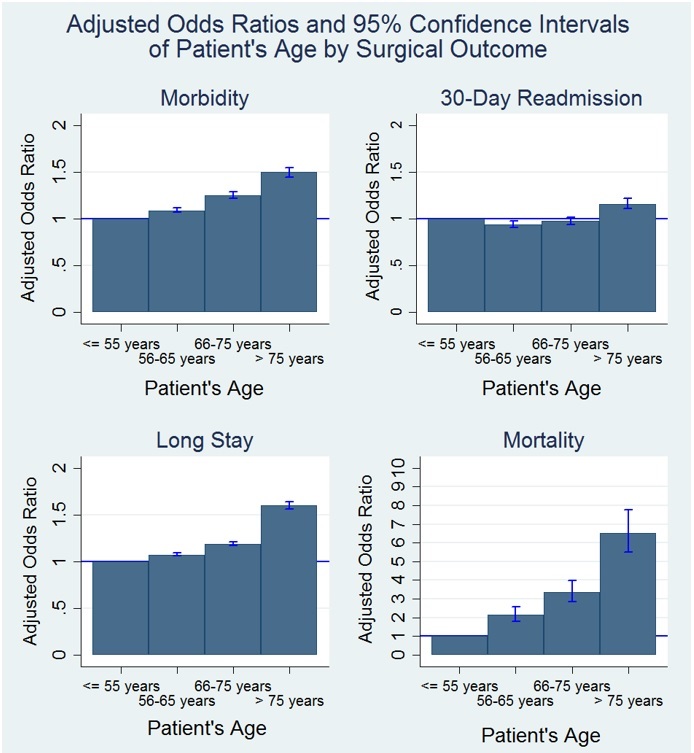
Objective: An increasing proportion of surgical patients are over the age of 65, and they are undergoing increasingly more complex surgical procedures. Prior studies have suggested that elderly patients are at increased risk of many surgical complications. We sought to determine whether the current effect of age on postoperative outcomes could be explained by increasing surgical complexity. Study Design: Multivariable logistic regression analyses were performed using high-quality clinical data for 676,953 patients from the 2015 National Surgical Quality Improvement Program (NSQIP) Participant Use File. Event rates of five surgical outcomes –postoperative morbidity, mortality, 30-day readmission, unplanned reoperation, and extended length of stay (LOS) (if LOS > 75 percentile within procedure group) -- were compared across four age groups (≤ 55 years, 56-65 years, 66-75 years, and > 75 years) accounting for patient-level covariates. Low-, medium-, and high-complex surgeries were defined by physician work relative value units (0-15, 16-25, and > 25). For each outcome, two logistic regression models were fitted to estimate the age main effects, with or without adjusting for surgery complexity. Population Studied: All elective surgical admissions within the 2015 NSQIP database were included. Principal Findings: After adjusting for patient-level covariates, including frailty, increasing age remained an independent strong predictor of increased morbidity, mortality, 30-day readmission, and extended LOS. Compared to patients ≤ 55 years, those above 75 years were 43% more likely (Odds Ratio (OR) = 1.43, 95% Confidence Interval (CI) = 1.38-1.47) to have any postoperative complication, five to six times more likely to die (OR = 6.20, 95% CI = 5.22-7.37), 12% more likely to be readmitted within 30 days (OR = 1.12, 95% CI = 1.07-1.17), and 53% more likely to have an extended LOS (OR = 1.53, 95% CI = 1.50-1.57). After adjusting for surgical complexity, increased age remained independently and significantly related to increased morbidity (OR = 1.50, 95% CI 1.45-1.55), mortality (OR = 6.53, 95% CI 5.49-7.76), 30-day readmission (OR = 1.16, 95% CI 1.11-1.22), and an extended LOS (OR = 1.60, 95% CI 1.56-1.64). Unplanned reoperation was not associated with increased age before or after adjusting for surgery complexity. Conclusions: Older patients continue to experience a higher risk of adverse surgical outcomes, including increased morbidity, mortality, extended LOS, and 30-day readmission. This effect was not mitigated by increasing surgical complexity. Implications for Policy, Delivery or Practice: With the aging population, additional resources and attention should be given to older surgical patients, particularly those older than 75 years of age. In addition, age-related surgical risk needs to be assessed prior to elective surgical procedures and communicated to patients.