Presenting Author:
Alysen Demzik, B.S.
Principal Investigator:
Department:
Orthopaedic Surgery
Keywords:
femoral stem length, EBRA-FCA, total hip arthroplasty, THA, PROMIS
Location:
Ryan Family Atrium, Robert H. Lurie Medical Research Center
C72 - Clinical
Femoral Stem Length Effect on Subsidence and Outcomes Following THA
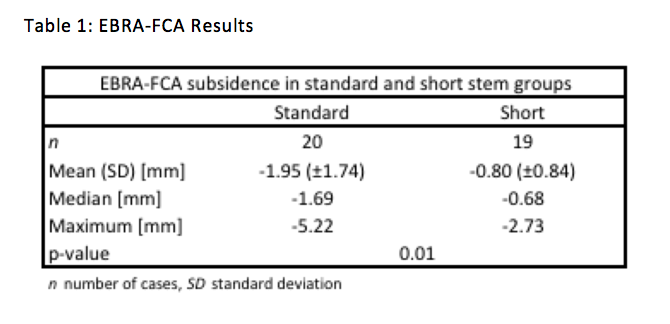
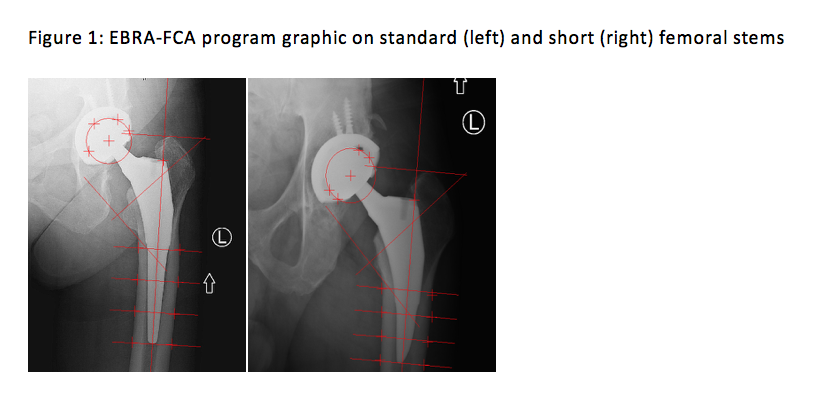
Introduction: Short stems have grown in popularity in total hip arthroplasty (THA) due to positive early clinical results and subsequent expansion of short stem indications, however clinical and radiological long-term performance has not yet been established. Implant migration following THA is an important factor in predicting implant survival in the long-term. Stems with axial subsidence rates greater than 2.4mm within the first two years are reported to be at high risk of failure. Early migration can be measured by EBRA-FCA (Einzel-Bild-Roentgen-Analyse-femoral component analysis), a radiographic analysis technique shown to be accurate and reliable that measures only comparable pairs of films to detect stem micro-movement. To date, there are very few studies comparing the migration of femoral short stems and traditional long stems. The purpose of this study is to assess the impact of femoral stem length on both clinical and radiographic outcomes of THA. Methods: We performed a prospective, randomized, blinded study comparing short and standard femoral implants of the same design and manufacturer. 57 patients undergoing THA were randomized into two groups at the time of surgery (27 short stems, 30 long stems) and all patients were made weight bearing as tolerated immediately following surgery. Patient demographics, radiographs, Veterans Rand 12 (VR-12) and Patient Reported Outcome Measurement Information System (PROMIS) were prospectively collected at 6 weeks, 3 months, 6 months, 12 months and 24 months. EBRA-FCA using standard radiographs was performed by a blinded technician to measure stem subsidence. Results: The average age of patients was 60 (30 females, 27 males) with no statistical difference in age (p=0.77), race (p=0.12), ethnicity (p=0.12), or gender (p=0.79) between groups. There was no difference between short and standard long stem groups in VR-12 mental (p=0.15-0.87) or physical component (p=0.33-0.77), PROMIS Physical Function (p=0.20-0.96), Pain Behavior (0.12-0.99) and Pain Interference (p=0.12-0.63) scores. The EBRA-FCA of 39 patients showed a mean subsidence of 0.80mm ± 0.84 for short stems and 1.95mm ± 1.74 for long stems p=0.013. No stems were revised for aseptic loosening and no stems were considered radiographically loose. Conclusion: This randomized trial showed no difference in clinical outcome between short and standard stem lengths. While both short and long stems had minimal subsidence, short stems were observed to be significantly more stable from time of implantation to latest follow-up.