Presenting Author:
Zachary Smith, M.D.
Principal Investigator:
Zachary Smith, M.D.
Department:
Neurological Surgery
Keywords:
Cervical spondylotic myelopathy, CSM, myelopathy, spasticity, spine
Location:
Ryan Family Atrium, Robert H. Lurie Medical Research Center
C56 - Clinical
Quantitative magnetization transfer MRI metrics in cervical spondylotic myelopathy
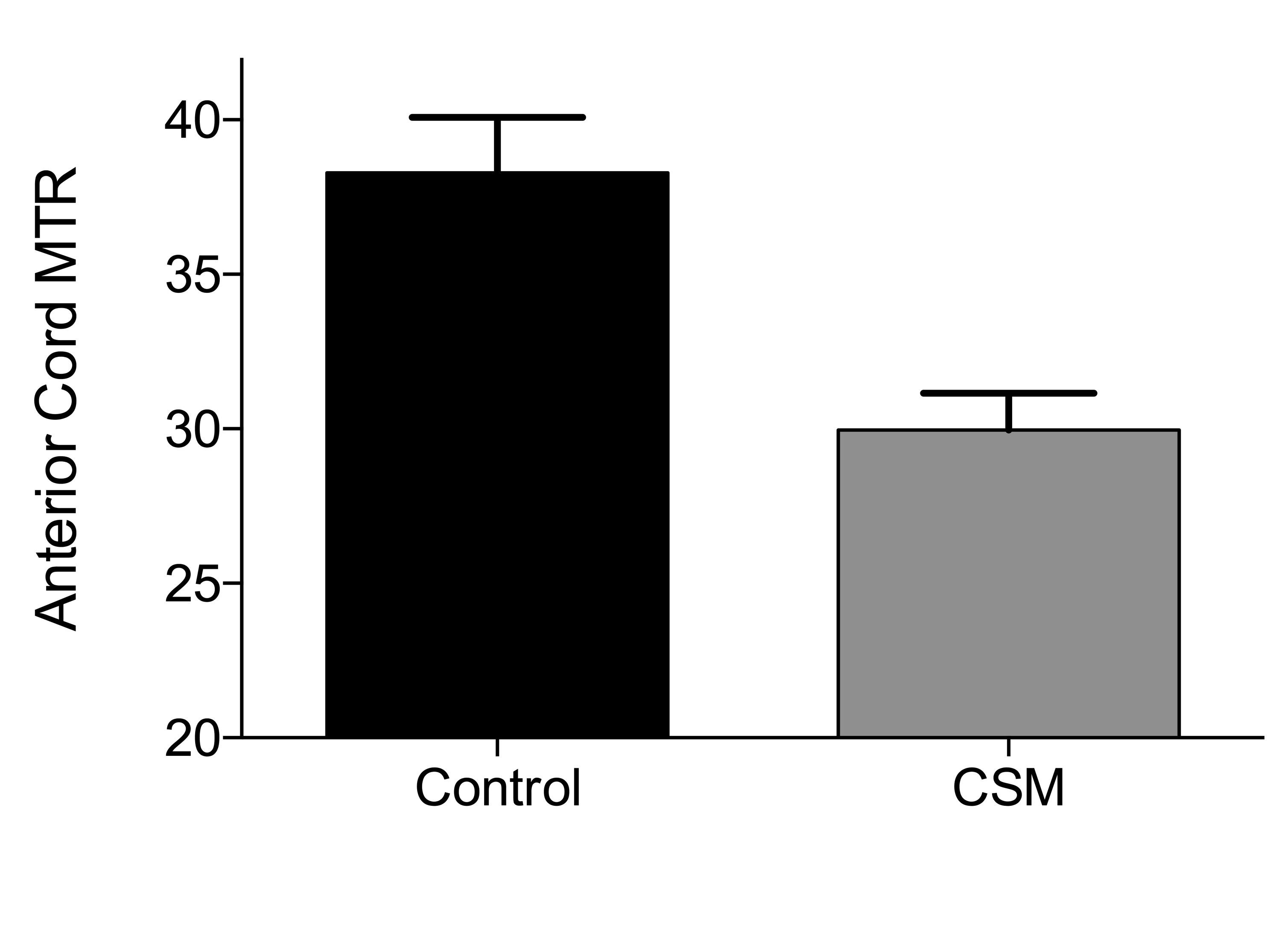
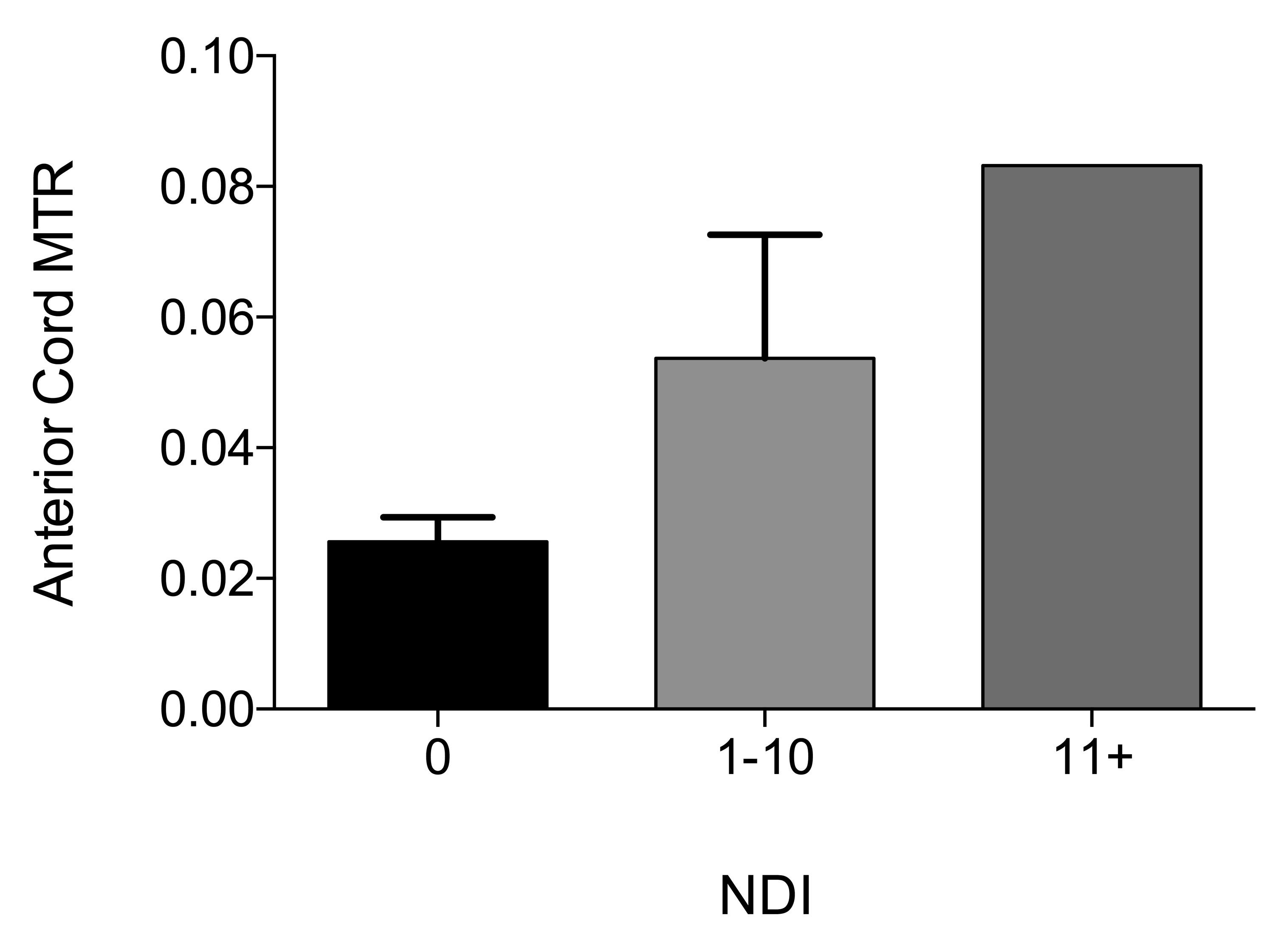
Background: Magnetization transfer ratio (MTR) is a quantitative measure that correlates with myelin loss and neural tissue destruction in a variety of neurological diseases. For example, in patients with multiple sclerosis, MTR of white matter lesions may predict clinical disability. However, the usefulness of MTR in patients with cervical spondylotic myelopathy (CSM) has not been examined. Methods: We prospectively enrolled seven CSM patients and seven age-matched controls to undergo MRI imaging of the cervical spine. Nurick, Neck Disability Index (NDI), and modified Japanese Orthopedic Association (mJOA) scores were collected for all patients. Clinical spasticity was tested at the MCP joint, using a 6-axis load cell. Reflex was simulated by quickly moving the joint from maximum flexion to maximum extension (300 °/sec). Anterior, lateral, and posterior cord MTR measurements were compared to clinical outcomes. Results: Compared to controls, CSM patients had lower anterior cord MTR (38.29 v. 29.97, ∆ = -8.314, p=0.0022), and equivalent posterior cord (p=0.2896) and lateral cord (p=0.3062) MTR. Higher Nurick scores were associated with lower anterior cord MTR (p=0.0205), but not lateral cord (p= 0.5446) or posterior cord MTR (p=0.1222). Lower mJOA was associated with lower anterior cord MTR (p=0.0090), but not lateral cord (p=0.4864) or posterior cord MTR (p=0.4819). There was no association between NDI and MTR of the anterior (p=0.4351), lateral (p=0.7557), or posterior cord (p=0.9171). There was a linear relationship between spasticity and anterior cord MTR (slope = -117.3, R = 0.6598, p = 0.0379), but not lateral cord (p=0.1906, R=0.4511) or posterior cord (p=0.2577, R=0.3957) MTR. Conclusion: Anterior cord MTR correlates with clinical outcomes as measured by mJOA index, Nurick score, and quantitative spasticity. Anterior cord MTR is associated with clinically relevant spasticity, and could play a role in the preoperative assessment of CSM. Understanding this radiological metric may refine surgical decision-making. Learning objectives: To understand the role of magnetization transfer ratio in identifying patients with clinically significant myelopathy and disability.