Presenting Author:
Jackson Herzog, B.A.
Principal Investigator:
Department:
Medicine
Keywords:
Medical student education, quality metrics, longitudinal, primary care.
Location:
Third Floor, Feinberg Pavilion, Northwestern Memorial Hospital
E14 - Education
Impact of a Longitudinal Medical Student Education-Centered Medical Home on Quality Metrics
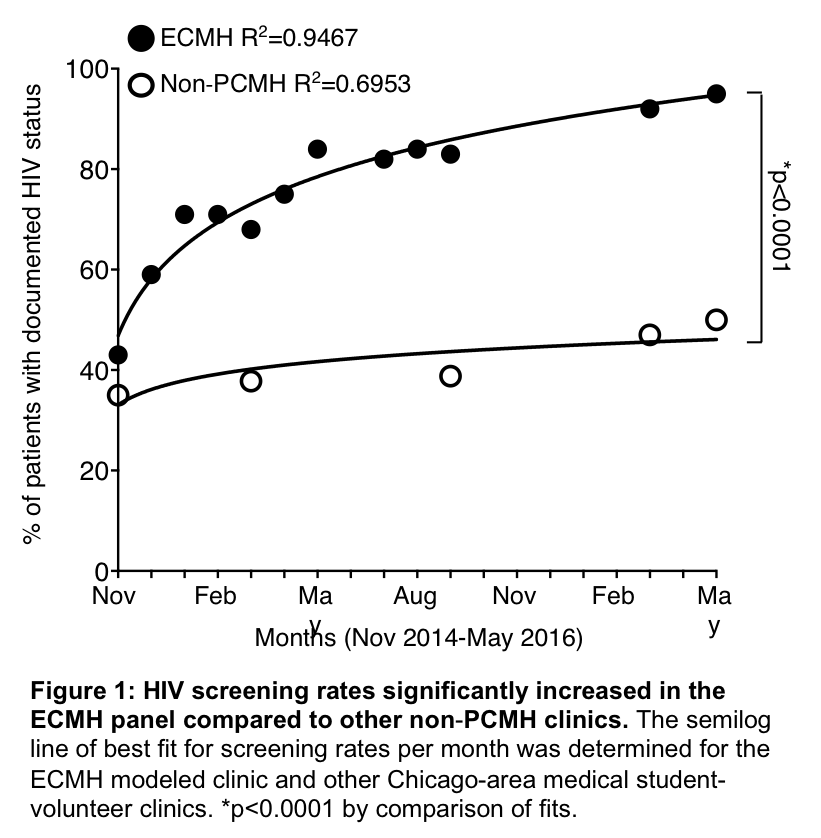
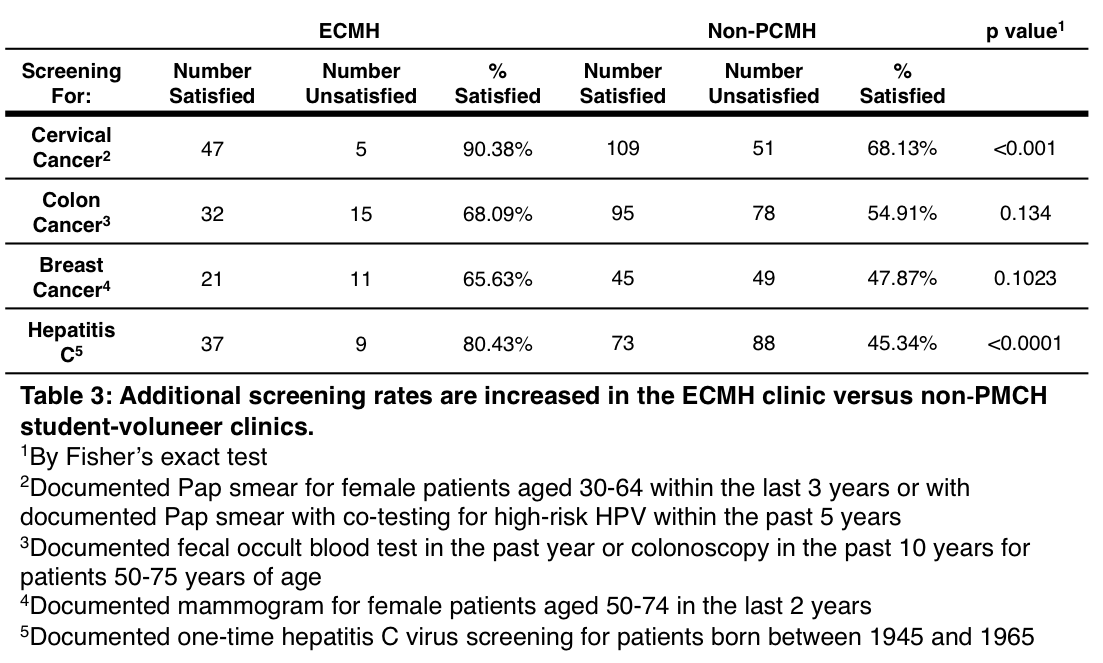
Purpose: Incorporation of the Patient Centered Medical Home model through longitudinal clinical clerkships is increasing in medical school curricula across the nation. While several studies document its benefit to the medical student experience, few have explored its effects on patient quality metrics and outcomes. Northwestern University’s Feinberg School of Medicine’s (NUFSM) Education-Centered Medical Home (ECMH) program is a longitudinal primary clerkship based on the PCMH model. Medical students work with the same attending physician, peer group and clinical staff at the same site to provide care to a consistent patient population across all four years of their training. In this study, the authors compare the impact of the ECMH model on HIV and other screening rates to the non-ECMH clinics at a student-volunteer free clinic (SVFC). Method: In September 2014, NUFSM converted its SVFC at CommunityHealth to an ECMH model. In accordance with ECMH principles, the students executed a quality improvement (QI) project to increase HIV screening rates. The proportion of patients with documented HIV screening was recorded after establishment of the ECMH model. It was then compared to the proportion of screened patients followed by four other non-ECMH SVFCs located at CommunityHealth. Percentages of patients screened for breast, cervical, and colorectal cancer, as well as hepatitis C, were also compared. Results: After adoption of the ECMH model, HIV screening rates increased from 43.2% (16/37 patients) to 95.0% (76/80 patients). This was a significant increase (p<0.0001) compared to the non-ECMH clinics. The proportion of patients successfully screened for cervical cancer (p<0.001) and hepatitis C (p<0.0001) was also significantly increased in the ECMH-modeled SVFC. Conclusions: These findings demonstrate that a student-led QI project in a ECMH-modeled SVFC significantly improved patient quality metrics compared to non-ECMH SVFCs. We hypothesize that the ECMH model improved continuity of care between students and their patient panel, and this enhanced continuity positively impacted the quality of care delivered. Future studies should examine the effectiveness of the ECMH model on more complex patient outcomes and different clinic structures.