Presenting Author:
Mansooreh Eghtesad, M.D.
Principal Investigator:
Luis Blanco, Jr.
Department:
Pathology
Keywords:
Pregnancy, Pregnancy-associated breast cancer, breast carcinoma, BRCA
Location:
Ryan Family Atrium, Robert H. Lurie Medical Research Center
C78 - Clinical Women's Health Research
Correlation of Clinical and Pathologic Features in Pregnancy-Associated Breast Cancer
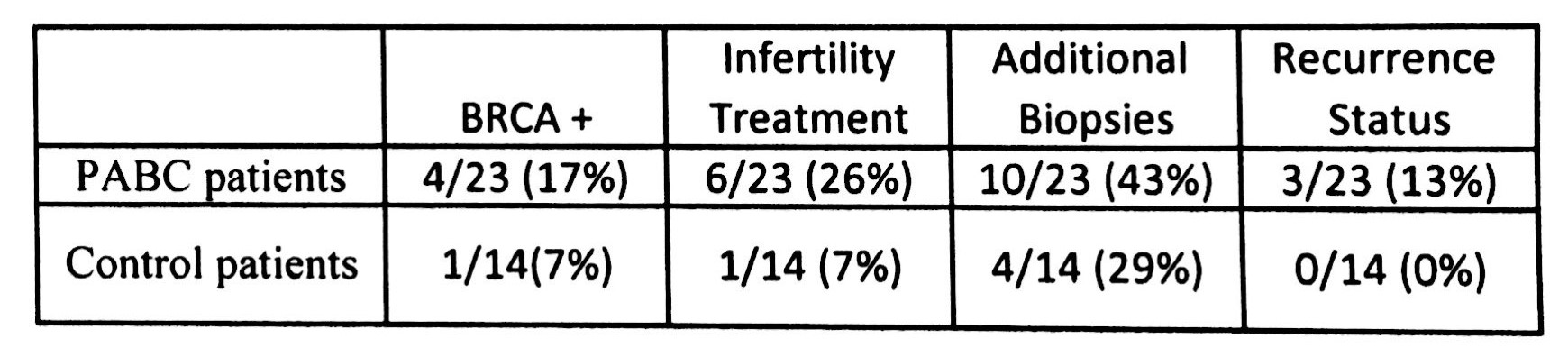
Background: Pregnancy-associated breast carcinoma (PABC) is carcinoma diagnosed during gestation or within 5 years postpartum and is associated with a poor prognosis, which is worse when diagnosed within 2 years of parturition. While previous studies have shown a unique set of pathologic features related to this subset of tumors, including higher tumor grade and associated inflammatory response, few have looked at the associated clinical aspects of these tumors. In this study, we analyzed clinical findings and correlated them with pathologic features to determine the impact that clinical factors have on PABC prognosis. Design: Twenty-three patients with PABC diagnosed within 2 years of pregnancy (mean age=35.8 years, range=26-48) and 14 control age-/stage-matched nulliparous women (mean age 37.5 years, range=29-51) were evaluated. Slides were previously reviewed and pathologic and immunohistologic tumor characteristics were recorded. The electronic medical records were then reviewed and clinical features including BRCA status, history of infertility treatments, additional biopsies and local/regional or distant recurrence were recorded. The average follow-up was 83 months (range=70-106 months). Results: PABC patients had a higher rate of BRCA-positivity (4/23, 17%) and infertility treatments (6/23, 26%) compared to matched controls (table 1). Interestingly, of the 6 PABC patients with infertility history, 2/6 (33%) had low grade (grade 1) tumors, while none of the other PABC patients presented with low grade tumors (0/17, 0%) (p=0.059). PABC patients also had higher rates of additional biopsies on follow-up and higher rates of tumor recurrence. No significant correlation was observed between clinical features and lymphovascular space invasion, lymph node positivity, or hormone receptor/HER2 status. Conclusion: PABC patients had higher rates of all clinical features assessed and had a worse prognosis on follow-up. Yet, PABC patients who underwent infertility treatment were more likely to have low grade tumors. Our findings suggest that aspects of the patient’s clinical history, as well as pathologic and immunohistologic characteristics, may influence the overall prognosis for PABC patients.